Wednesday Bubble: is DHEA the path towards a better sex life?
Today’s Bubble is a doozie that can one of two ways: in the yes(!) column or in the no (!) column. I’ll leave it to you to decide.
DHEA is the most abundant sex hormone in circulation and is mostly secreted by the adrenal glands. Research has shown that low DHEA levels in pre- and postmenopausal women may negatively affect sexual functioning, while ample blood levels may enhance sexual functioning, cognitive functioning and wellbeing. Yet, whether or not DHEA really works continues to be controversial. And the reason behind the burgeoning interest is the quest to find a suitable replacement for HRT. The thing is? There are lots of suitable, evidence-based replacements that are not broadly accepted by many medical professionals and many of these are discussed regularly on this blog. Nevertheless, here’s what researchers have just discovered about DHEA.
The researchers, from Pisa, Italy, followed 48 healthy, postmenopausal women for a year. During this time, they divided 36 women who were experiencing troublesome menopausal symptoms and requesting hormone replacement into three groups:
- 12 women who received 10 mg daily of DHEA
- 12 women who were given combined HRT
- 12 women who received the synthetic hormone, tibolone, daily
The fourth group was comprised of 12 women who did not wish to use HRT. They received daily vitamin D (400 IU) and calcium to help combat osteoporosis.
At the start of the study, all of the women reported similar sexual activity. However, after a year of treatment, women taking DHEA had significant increases in sexual interest and activity scoring almost 14 points higher on a questionnaire used to measure sexual interest, satisfaction, vaginal lubrication, orgasm and sexual partner. The women taking HRT experienced similar benefits, and women in both of these groups reported engaging in more sexual intercourse compared to women taking Vitamin D and calcium. Women taking the synthetic hormone also had increased sexual interest scores but they were not as high as the other two hormone groups. The magnitude of improvements in menopausal symptoms was also similar between the DHEA, HRT and tibolone groups.
The reason for this improvement appears to be the effect that DHEA has in terms of improving blood levels of the hormones estradiol and progesterone, both of which decline during menopause. It also appears to positively affect adrenal functioning.
What to think? Well, the study didn’t include any information on side effects. This is what Mayo Clinic has to say in that regard:
“No studies on the long-term effects of DHEA have been conducted. DHEA can cause higher than normal levels of androgens and estrogens in the body, and theoretically may increase the risk of prostate, breast, ovarian, and other hormone-sensitive cancers. Therefore, it is not recommended for regular use without supervision by a licensed health professional.”
Another important fact, acknowledged by the researchers, is that DHEA was only studied in 12 women, hardly enough to draw any firm conclusions. But they do believe that the findings, albeit preliminary, are encouraging, especially for women who “may have problems in taking more conventional HRT.”
Personally, I believe that it’s waaaaay too early to even consider DHEA as an alternative to HRT and in particular, to androgen therapy for sexual health. I want to see more information on side effects before it’s even on the radar. Meanwhile, I would love to hear what you think:
Yes!?
or,
No!?
Read MoreGuest Post Roundup: Sex, Generations and A Whole Lotta Love
As we come closer to the year’s end, I’d like to express my gratitude to a few of my colleagues who took the time to publish their thoughts on Flashfree this year. And, althoughI receive a lot of solicitations, there are few that I feel are worthy of your time or your close read. These, on the other hand, rocked my world, not only because of their breadth and finesse but also because of the love behind the words and thoughts.
This is a Roundup that you don’t want to miss.
[Credit: Special and enduring thanks to artist Darryl Willison of whimsicalwest.com. Please visit his site and support his work!]
- Should fatties get a room? Dr. Brian Hughes has lent his fine prose to this blog several times and often writes insightfully about how our society takes advantage of women. When I stumble across something on his blog that screams Flashfree, I reach out and say pretty please. Brian rocks!
- Should I or shouldn’t I? Oncologist, journalist and educator Dr. Elaine Shattner has spent most of her online bandwidth on discerning the facts about breast and other cancers. Let’s face it; there is a lot of information swirling around the Interwebz and when it comes to figuring out what it means, well, the challenge can be daunting. Want to know more? Elaine’s your girl for the 4-11.
- Anti Anti-Aging, Pro Great Glow. Do you want to fight your years? Or fight FOR them? Writer and author D.A. Wolfe dishes up some provocative prose and challenges the inner you. This one’s got “win” written all over it.
- Counterterrorism, women and 9-11. Doesn’t sound like a topic for Flashfree, does it? But my friend Anne Weiskopf shares a poignant piece about what it means to be a woman. And a mother.
- Want to get your groove on? Move. Alexandra Williams, motivational speaker, fitness writer, radio host and inspirateur nails it with a wonderful post on sex, exercise and wellbeing.
- Vagina’s are like self-cleaning ovens. Wait! What?! Yes, gynecologist and sex expert Dr. Jen Gunter makes a guest appearance to shake up the idea that douching is a good idea.
- Have you crossed the Big M finish line? Author Sarah Bowen thought she had. And tells us how she hit the reset button before the race ended.
- On Becoming Bendy. Author Patti Digh is at it again. She’s changing our world, one day at a time. And wow, has she ever changed hers’ this year. Want to be a better you? Bendy. Who said that Gumby didn’t have an alterior motive?
- Are you becoming your mother? When was the last time you looked in the mirror and asked yourself the very question that my friend, motivational speaker and author Cherry Woodburn asks in this post? Are you a generational profiler?
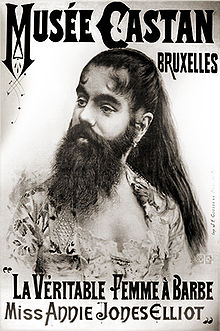
Hairy kiri…sexual desire and hairs on your chinny chin chin
Yes, I am taking poetic license with the Japanese term “Hara-Kiri” which literally means to cut or slice the stomach. This phrase has been hijacked by slangers who refer to it as ‘hari kari,’ to off oneself or commit suicide.
I propose that using testosterone in hopes of improving sexual desire is a great way to cut off one’s wellbeing and sense of self Chi, leaving hairs on the chinny chin chin and other undesirable locations.
Hairy kiri? You bet!
Back in 2008, I wrote about Intrinsa, a testosterone patch that was tested in a study of 841 postmenopausal not currently on hormone replacement therapy to test its effects on sexual desire after about a half a year’s use. The results, which were published in the New England Journal of Medicine, showed that compared to a dummy patch, using low or high dose Intrinsa was associated with significant increases in sexual desire and a decline in sexual distress. Overall, the higher dose patch led to modest improvements in sexual function. In other words, wearing a patch was significantly better than using nothing at all but not life-shattering in terms of improving sexual function. However, the caveat was unwanted hair growth, which occurred in about a third of women using the higher dose patch and in about 23% of women using the lower dose.
Once I delved further into androgens and women, I learned that while it has been suggested that local circulating levels of androgens are associated with low sexual desire and sexual dysfunction, the data are contradictory. Moreover, in a fairly recent scientific review, researchers say that no single androgen predicts which women will have sexual dysfunction, making it even harder to address, right? What’s more, they also note that laboratory studies have only limited value and aren’t routinely recommended.
Looking more closely at different formulations of androgens like testosterone, e.g. patches, oral tablets, implants and injections, experts have found that the major side effects are unwanted hair growth and acne. Both are related to dose and how long treatment lasts, and disappear once treatment is stopped. And while rates of hair growth are definitely lower for patches in general (as few as 7% to as high as 23%), as many as 36% of women who use oral testosterone have unwanted hair growth. Among those receiving implants, pellets or injections the number is also high: 20%.
Let’s face it; the trouble is testosterone is that it may only address a miniscule amount of factors affecting a woman’s libido and in literally leave a trail in its place. Don’t know about you but I think it’s a hairy kiri proposition. A few more notches on the desire scale and a few more hairs in your chin, on your chest and lord knows where else.
Committing hairy kiri ain’t for sissies; that’s for sure!
Read More
Wednesday Bubble: Are you in the moo? Sex and a sense of purpose
What are we bursting this week? How about midlife and sexual desire. Frankly, I’ve got sex on the brain, sex in midlife, that is. And what we need to do to insure that it continues to be enjoyable, that we desire it and that we please our partners as much as we hope that they please us. Consequently, I am reposting this piece from earlier in the year, with the hope that with a sense of purpose, you’ll become more in the moo. Or mood. Whatever the case may be.
Sexual desire. In midlife, sexual function and sexual desire aren’t well understood, primarily because there are so many factors that enter into equation. This may be why certain silver bullets, like a female viagra, has failed to show any significant improvements in the desire department. And yet, researchers continue to accrue more information about the things that influence desire in women, ranging from the quality of intimate relationships to social support and overall wellbeing. The manufacturer who discovers a pill that addresses all of these will have struck gold. Meanwhile, back in reality, as many as 75% of women in midlife rate sexual health as important enough to warrant further exploration.
Fortunately, we may have another piece of the puzzle: ‘sense of purpose,’ which appears to be associated with greater wellbeing, happiness, life satisfaction, self-esteem, personal growth and optimism. A sense of purpose also appears to improve health, prevent certain diseases and may even improve cognitive function, thereby staving off mental diseases associated with aging. In a study that appears in the online version of Menopause, 459 menopausal women who were sexually active with a partner were followed over three years. Each year, they were asked about their emotional wellbeing (including their general mood, anxiety and depression as well as how often they engaged in and enjoyed sexual activity (specifically desire, type of activity and hugging and kissing). In the final year, they took a test that rated their sense of purpose on a five point scale ranging from ‘there is not enough purpose in my life’ to ‘the things I do are all worthwhile.’
The findings?
A greater sense of purpose equaled a great enjoyment of sexual activities, independent and regardless of other specific life circumstances. In other words, psychosocial functioning, e.g. social support, quality intimacy and overall wellbeing influenced the quality of these women’s sexual lives. On the other hand, menopausal status and use of hormone therapy did not appear to play a significant role in how often women engaged in sex or if they enjoyed it. This is important, as it means that psychosocial wellbeing may ultimately be more important than hormones.
In so far as the desire to engage? Women who were younger, had more social support, felt better about themselves and weren’t suffering from vaginal dryness tended to want sex more than their older peers who didn’t enjoy these factors.
Not surprisingly, many of the factors that researchers stress may help desire and engagement are associated with greater nitric oxide levels, which Dr. Christina Northrup says can help combat sexual dysfunction and improve pleasure.
When it comes to sex in midlife? It may help to think ‘sense of purpose,’ a real sense of purpose, now. (Poetic license, Chrissie!) I’m all for it if improves activity and desire without drugs.
Read MoreWednesday Bubble: More on maca – not ready for prime time
Remember maca? The aphrodisiac of the Andean plains that is even used in fjords of Norway? When it comes to menopausal symptoms and female hormonal balance, it seems that maca is not all it’s cracked up to be. In fact, before you spend your hard earned dollars on this Andean wonderherb, you may want to hear more.
In case you are unfamiliar with maca, it is a plant indigenous to South American countries that has been used for centuries by Peruvians and other cultures to manage conditions such as anemia, infertility and as mentioned, hormonal imbalances in women. More recently, it’s been introduced in Europe, the US and Asia as a potential treatment for impaired sexual function and desire.
However, despite its touted benefits and burgeoning marketing buzz, maca may not be “all that.”
In the scientific world, researchers often look at published studies and data in composite in order to evaluate the effectiveness or worthiness, if you will, of a product or strategy. These efforts are call meta-analysis, and consist of culling, pooling and then evaluating information that was collected over certain time periods. Importantly, when they tried to do this with maca, searching 17 international databases for studies up to June of this year, they discovered the evidence was lacking, forcing them to synthesize or qualitate what they were able to find based on the strength of the evidence that did exist. In summary:
- Out of 17 scientifically rigorous studies that they were able to locate, only four held up to standards and therefore, worthy of inclusion.
- In total, 202 healthy pre- or post-menopausal women took pre-gelatinized or dried commercial maca or placebo, in different doses (1.0 to 3.5 gram daily) for up to 2 months.
- Various menopausal symptoms were studied using scientific indices. They ranged from vasomotor and mental health to sexual dysfunction and overall wellbeing.
Although three of the four studies showed that maca had positive and even significant effects on menopausal symptoms compared to placebo, the researchers emphasize that “perhaps the most important finding of this systematic review is that there have been very few rigorous trials examining the effects of maca on menopausal symptoms.” Given that maca has been marketed as effective for the treatment of menopausal symptoms, they find the lack of data surprising. Moreover, the studies were so disparate in terms of how maca was used that it’s difficult to draw any worthwhile conclusion about its effectiveness. In fact, the optimum amount of maca is still not known.
Tell me, how can you treat your symptoms effectively if you don’t know what dose to use?
Experts also don’t know how maca works; theories include that it may stimulate the production of estrogen or that it fortifies the body’s ability to maintain hormonal balance. Nevertheless, others argue that despite the clear evidence, maca appears to cause fewer side effects than conventional drugs for menopause. In fact, none of the studies examined in the review showed any adverse events (some claim that there are no reports of adverse effects whatsoever, although Peruvian authorities recommend that it is boiled before consumption to insure safety, and Australian authorities report attention disturbances, weight loss, agitation, nausea, vomiting, abnormal liver function, abdominal pain and oral tissue bleeding). The reason it’s so important to clarify this particular safety profile is that if maca has an estrogen effect, it might be contraindicated in women with conditions that are sensitive to estrogen, such as endometriosis and breast cancer.
The bottom line is that we need more scientific studies and a heck of a lot more information. Meanwhile, although it’s definitely affordable (a quick Google search shows that pricing per bottle or in bulk ranges from $4 to $23), there doesn’t seem to be enough evidence to support regular use of maca for menopausal symptoms and sexual function. This is definitely a path wrought with lots of questions. Buyer beware. Maca isn’t ready for prime time, at least not yet.
Read More
Wednesday Bubble: Exercise and Sexual Health – How you move affects how you groove. Guest post by Alexandra Williams, MA
Every now and then I like to shake things up in this space, which is why I asked fitness professional writer, speaker and radio host Alexandra Williams (aka @alexandrafunfit on Twitter) to lend me her expertise for a day. What I didn’t expect, however, was for her to rock the sexual health world with the revelation that exercise, i.e. how you move, affects how you groove. Frankly, if all it takes is exercise, you will find me adding an extra hour or so a day at the gym!
Show Alexandra some love. She’s witty and has been putting the fun back into fitness for for some time now…
Image: http://vectorportal.com
Sexual health is defined by Mosby’s Medical Dictionary. as “a capacity to enjoy and control sexual behavior without fear, shame or guilt.” Sexual dysfunction is broadly defined by the Gale Encyclopedia of Medicine as “disorders that interfere with a full sexual response cycle. These disorders make it difficult for a person to enjoy or to have sexual intercourse.”
The good news, especially for older adults, is that most sexual dysfunctions can be treated or alleviated through exercise. It has been found to increase sexual drive, functioning, activity and satisfaction, due to the physical endurance, muscle tone and body composition derived from exercise. In addition, exercise activates the sympathetic nervous system, which encourages blood flow to the genital regions. Even low levels of physical activity can elevate mood and help keep sex organs and muscles in better working condition. A 2000 study found that after just 20 minutes of vigorous exercise, women became more sexually responsive, while men had increased testosterone levels after short, intense bouts of exercise.
Frequency, level of desire, and enjoyment are also affected positively for those who engage in regular exercise, at any age. In 2004, a study of college-age students a strong correlation was found between fitness levels, self-perception, body image, social meaning, outward appearance and sexual performance and desire. These findings were replicated in studies of people in their forties and sixties. And of course, sexual activity itself counts as exercise!
One really interesting comparison of exercise and sexual activity, looked at heart rate and blood pressure during treadmill exercise and sexual activity (not simultaneously)! Unsurprisingly, participants spent more time in sexual activity than they did on the treadmill, but here’s the intriguing point – the treadmill exercise duration predicted sexual activity duration. For each minute of treadmill time, there was 2.3 minute increase in sexual activity duration!
There are also a number of sexual diseases and dysfunctions that are radically improved through exercise. For example, exercise has a protective effect on Type 2 diabetes, with pelvic floor exercises of specific value. A minimum of approximately 50% of overweight men with Type 2 diabetes have erectile dysfunction, a frustrating condition that is helped enormously by cardiorespiratory fitness.
Urinary incontinence is markedly improved via pelvic floor muscle training, with 100% of women reporting decreased incontinence frequency and duration. And it works for men too – after the strengthening training, incidences of urinary and fecal incontinence decreased, and erectile function increased. Pelvic floor exercises are also an effective modality for primiparous (giving birth only once) women who have vaginal deliveries. Desire and satisfaction go up, and pain goes down for these women.
Breast cancer survivors consistently report an improved quality of life (better physical functioning, reduced fatigue and pain) when they participate in physical activity. In addition, prostate and bladder cancer are positively affected by exercise, including its stress-reducing aspects.
Sexual activity itself has been found to help with cardiovascular disease, with researchers finding that sexual activity corresponds to light to moderate physical exercise and entails no significant risk to the majority of patients with cardiovascular disease (severe angina or chronic heart failure are exceptions).
There’s been a lot of research on the relationship between exercise and erectile dysfunction, which affects over 100 million men. The link between cardiovascular disease, metabolic syndrome and erectile dysfunction is strong, and exercise is a mitigating factor on all three. Doctors who prescribe movement to patients with these three issues have reported high success rates. This is good news, especially considering that exercise is a less invasive treatment than medications, surgery or testosterone replacement therapies.
Sexual functioning and health is something everyone should have at any age. Exercise just may be the magic pill!
About the author…
Alexandra Williams, MA, has been in the fitness industry for over 25 years. She is the co-owner of funandfit.org. Together with her twin sister, she writes, teaches and speaks on fitness-related topics, using wit and research! For more, be sure to write to Alexandra and Kymberly at info@funandfit.org.And if you are the sort of person who likes to put a voice to an image, be sure to check Alexandra and Kymberly out on their radio program ‘Fun and Fit.’
Read More