Flashfree…time for a new journey
Hello there! I’ve been gone for about four years but I’ve been eager to get the site back up and running to provide women (and men) access to six some-odd years of posts and information. In the coming weeks, the site will be undergoing a revamp and slight change in direction, a new journey, if you will. While we would like to believe in the utopian fantasy that health is created equally, and that health needs are likewise, the same between women, data suggest otherwise. Women of color have increased rates of hypertension (aka high blood pressure), diabetes, death from breast cancer, etc. And as you may know, menopause is a prime time for the body to go haywire and certain disease risks, elevate markedly. So, stay tuned as I have a few thoughts about devising content that is specific to women of color, in addition to content that applies across the gender spectrum.
Blogging may be dead. However the search for current information never goes away.
Welcome back!
Read MoreRevisiting up in smoke…
I remember the first time I had a cigarette. It was a Kool, purchased surreptitiously from the candy shop across the street from McKinley School. The year was 1969 and I was eight years old.
Yes, I said eight!
It used to be cool to smoke. My girlfriends and I would pretend we were in the teachers’ lounge (remember those?). By the time I got to college, I switched to clove cigarettes. And then afterwards, Marlboro Lights. I was up to a pack and a half a day by the time I stopped smoking. At the age of 30.
This means that I smoked, on and off, for 22 years.
At the age of 46, I had my first night sweat. I turned 52 this past May, and the sweats continue.
You may wonder why I’m sharing these intimate details of my covert and then overt smoking life, and my sweaty journey…
Researchers say that first- and second-hand smoking not only increases the risk for death from heart disease and cancer, but may also significantly increase the risk for starting menopause at an earlier age (i.e., around age 45 rather than the average age of 51).
Data from a cross-section of 5,029 women aged 25 and older participating in the National Health and Nutrition Examination Survey III have shown that women who were current smokers (as measured by self-reports and blood levels of nicotine) started menopause at a mean age of 47, while women in service industries who were exposed to nicotine in their jobs started menopause at a mean age of 46.
Black women who had been regularly exposed to cigarette smoke had 12 times the odds of other racial groups of an earlier menopause age compared with smokers and nonsmokers who had not had any exposure. The investigators attributed this significantly increased risk among Black women to the body’s inability to clear nicotine from the blood as quickly as their peers.
The purpose of this study was to demonstrate that women in the workplace who are exposed to second-hand smoke are at increased risk for many of the same diseases as smokers. They’ve now added early menopause to this list.
What is less clear, however, is the risk for “former smokers,” since they were taken out of the analyses.
Makes you wonder if many of us who are former smokers or were exposed to second-hand smoke on a regular basis in our homes (a good percentage of women our age, as my sister in law pointed out), are at a higher risk as well.
Sort of like poster children, right?
It concerns me that a new generation of women who are into vaping might end up in the very same place that I and perhaps you did. It’s too soon to tell. However, time to put the myths to risk. Smoking not only kills but it may be setting you up for an early bout of sweats and flashes. Trust me, they’re not fun.
Read More
Don’t put all your eggs in one basket!
Back in 2010 I wrote a piece about a woman’s egg supply and its role in predicting when menopause may start. There’s some new information to add to the story so thought I’d rerun the piece with a few highlights.
So eggs and baskets. What, pray tell, do they have to do with menopause? Let’s break it down, step by step (or, year by year, as the case may be). The bottom line is that roughly 69% of the total reserve of eggs that a woman has and how that varies throughout her lifetime can be determined by age alone.
While still in the womb, a female will develop several million eggs. Up until age 14, the eggs will continue to increase in number, accelerate around puberty (i.e. ages 9 through and then the reserve steadily declines until menopause (around age 50 or 51).
Using computer modeling of data taken from about 325 women, researchers determined that by the age of 30, 95% of women will only have 12% of their egg reserves remaining. By age 40, only 3% remain. What’s more, age remains the primary influencer of the number of eggs up until about age 25. Then as a women grows older, other factors, including smoking, body mass index, stress and previous pregnancies start to play more important roles.
Back to the menopause component. The majority of readers of this blog are of the age where pregnancy is no longer a consideration an the number of eggs in reserve, pretty irrelevant. However, by considering and mapping how the ovarian reserve of eggs is established and then diminished in the first place, researchers hope to be better able to predict when menopause will start individual women. This strategy compliments the anti-Mullerian hormone blood test (check out information on that here) and closely follows the way that scientists used the blood test to predict menopause.
However, geeky science aside, by having a better idea of when menopause will start, you may be able to take appropriate steps in a timely fashion to both stave off vasomotor symptoms such as hot flashes and night sweats and maintain body weight and physical health. What’s more, imagine the possibilities in terms of mood swings and depression. The potential rewards are endless.
According to the researchers, they might also be able to predict which women treated for cancer are at highest risk for early menopause as the result of treatment. Since many of these women are young, this might provide opportunities for proactive family planning.
And finally, by measuring ovarian volumes, a key factor in the computer modeling, researchers believe that they may be able to predict young women who are at risk for developing premature loss of their ovarian function, a common side effect of cancer treatment. The benefit here is that it may be a way to help these young women preserve their eggs early for later fertility efforts.
So, all those eggs in one basket? You might not be able to control how many but you may be able to control certain outcomes. Nice!
Read MoreNewsflash! When it comes to symptoms ‘down there,’ does terminology matter?
GSM (genitourinary symptoms of menopause) is a new acronym being adopted by the North American Menopause Society (NAMS) and the International Society for the Study of Women’s Sexual Health (ISSWSH) to encourage dialogue between female patients and their doctors. NAMS says that it refers to the genital, sexual and urinary problems that make women and their doctors uncomfortable discussing. “Having a term that doesn’t carry stigma, isn’t embarrassing to say, and is medically accurate could go a long way in helping women get the help they need and allowing them to make smarter healthcare decisions.”
The vagina and surrounding area (e.g. urethra, lower end of the bladder) are estrogen and androgen receptor-rich. Hence, the decline in estrogen and other sex hormones during menopause can lead to thinning of tissue, loss of elasticity, dryness and physical changes that increase the risk for infection and discomfort. The issue with current nomenclature is that terms that have traditionally referred to genital problems that occur after menopause aren’t accurate; for example, atrophic vaginitis refers to inflammation and infection, both of which may not be the underlying issue during menopause. Atrophy infers that something is wasting away from disuse, which isn’t always the case; rather, pain and dryness can lower libido significantly. Additionally, previously used terminology pretty much ignores urinary problems like overactive bladder, stress incontinence and recurring urinary tract infections.
Yet, there is another part of this story; the stigma attached to the terms used to describe the issues. I’m not sure that I agree with the organizations’ claim that women are too embarrassed to use the term ‘vagina’ with their physicians; after all, when you are sitting in stirrups and the gynecologist is peering into your vagina and you have a question, do you refer to your privates as ‘vajayjay’ or ‘nether region?’ Perhaps prior generations have trouble using the ‘V’ word but as a child of the 60s and 70s (Our Bodies, Ourselves, anyone?!), I would hope that we would have gotten past the embarrassment by the time we reach menopause.
In a related press release, Dr. Margaret Gass, Executive Director of NAMS is quoted as saying that “GSM will make discussing the problems so much easier, similar to the way ED changed our ability to talk about impotence.”
I question the value in further stigmatizing an inherent and necessary part of the female anatomy. Are we still so archaic that in the 21st Century we need an acronym to avoid discussing sensitive issues?
From where I stand, the greatest benefit from this initiative will be to help women understand why these problems happen, that hormones are at-play. The organizations are also developing a tool to standardize aspects of a physical exam to look specifically for the types of changes that cause these issues in menopause. Those two things are wonderful. But do we need truly need another acronym, one that may actually prevent what I hope will be an evolution in thought and communication and the end to an arbitrary code of ethics?
Read MoreWacky menopausal function?
Try Ovazyl.
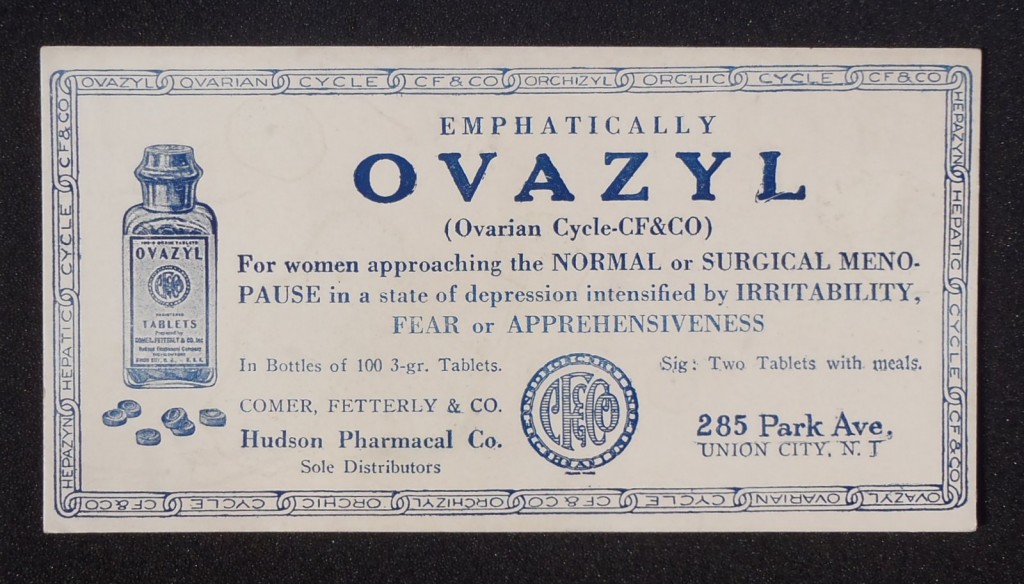
Described in the International Record of Medicine and General Practice Clinics (published 1922) as an endocrine functional tonic, Ovazyl was specifically (or “emphatically”) for women entering natural or surgical menopause in a “state of depression intensified by medical and physical irritability, fear or apprehensiveness.”
These nifty pills were developed from raw endocrine glands that were extracted and then dried up under laboratory conditions. Theoretically, two pills daily with meal would address ovarian or thyroid ‘weakness, menstrual disorders, neuroses and high blood pressure. The hormonal fountain of youth, if you will. Or something like that. The tricky part is replacing dwindling hormones with dried up glands rather than the hormones themselves.
Don’t know about you but raw endocrine glands are probably best with fava beans and a good chianti, if you get my drift.
Yikes! Another winning tonic from days of yore.
Read More
Evidence
A few weeks ago, I found myself in the midst of a discussion about the value of acupuncture for a variety of diseases. And I quickly realized that there was no value in continuing the dialogue as the person who had started the discussion had no interest in hearing anything but his own point of view.
This is commonplace in allopathic, or Western Medicine.
There is a word that is thrown around a lot in scientific circles: evidence. If something has not proven beneficial according to scientific standards that rely on a specific framework of measures, then it has no value. However, in my small circle, value is defined a bit differently and evidence, taken as a grain of salt because not everything can be explained away by science. Or by a clinical trial that creates an artificial environment to evaluate benefit. And practitioners who rely on nothing but this artifice, I posit that perhaps it is their patients who suffer the most, the reason being that even the standards aren’t truly standardized.
Several years ago, Mike Clarke from the School of Nursing and Midwifery at Trinity College in Dublin wrote a great article about the need to standardize results of studies for a specific disease ( in this case, rheumatoid arthritis). He defined the problem as follows:
“Every year, millions of journal articles are added to the tens of millions that already exist in the health literature, and tens of millions of web pages are added to the hundreds of millions currently available. Within these, there are many tens of thousands of research studies which might provide the evidence needed to make well-informed decisions about healthcare. The task of working through all this material is overwhelming enough without then finding the studies of relevance to the decision you wish to make…”
So what do you do? A few key points:
- Consider that every study has the potential for bias. Perhaps researchers are using 7 instruments to measure depression and only highlight findings from 3 of these in order to preserve the most positive or significant results. Clearly, the reader is being led towards certain outcomes and away from others. And regardless of what one believes, statistical analyses do not always reveal the truth.
- Study designs, types of patients studied, age of patients studied, gender, you name, can differ so it’s difficult, if not impossible to draw definitive conclusions when comparing results of one to another.
- Another issue of great interest to practitioner of Western medicine is whether or not a study is controlled. This means that two groups are compared that are identical in every way except one group is given an experimental treatment and the other, a placebo or standardized treatment. Note that often, real world conditions are often recreated rather than conducted in a real world setting and many studies are not controlled, meaning that the science behind the findings is questionable. And, what is often missing in these studies is the individualization of treatment – no one patient responds the same way as the other. Importantly, Eastern medicine recognizes this and adjusts treatment accordingly.
- I can’t emphasize this last point enough: alternative and complementary medicines are still incompletely understood among many practitioners of Western medicine. What’s more, agents are not regulated carefully and manufacturing practices may vary. Consequently, studies of these agents or modalities are often inconclusive. And of course, often underfunded and under-appreciated.
I’ve written several times about the importance of consulting a practitioner or medical expert before embarking on any regimen for peri- or postmenopausal symptoms. In fact, you should consult several and then compile the information to devise a plan that works best for you. You may need to try different combinations before you find the key to your individual health. Yet, if you only see someone once, at least that dialogue may be useful for initially defining a regimen that may work best for you and what you’re going through. For those of you who live off the beaten track without access to a good practitioner, excellent resources like Medline or the American Botanical Council may be be of help in discerning what’s what.
The short answer is that there are no short answers. But with careful guidance and a bit of prudence, you may just be able see the light and smooth out the bumps on this rollercoaster ride we’re all on.
Read More










