What’s it all about, Flashfree? The Lowdown on Estrogen
I spend a lot of time and energy discussing the role of estrogen in menopausal symptoms. However, it occurred to me recently that readers might not truly understand the distinction between pre and post menopause and how estrogen levels interact with the body to cause a host of issues.
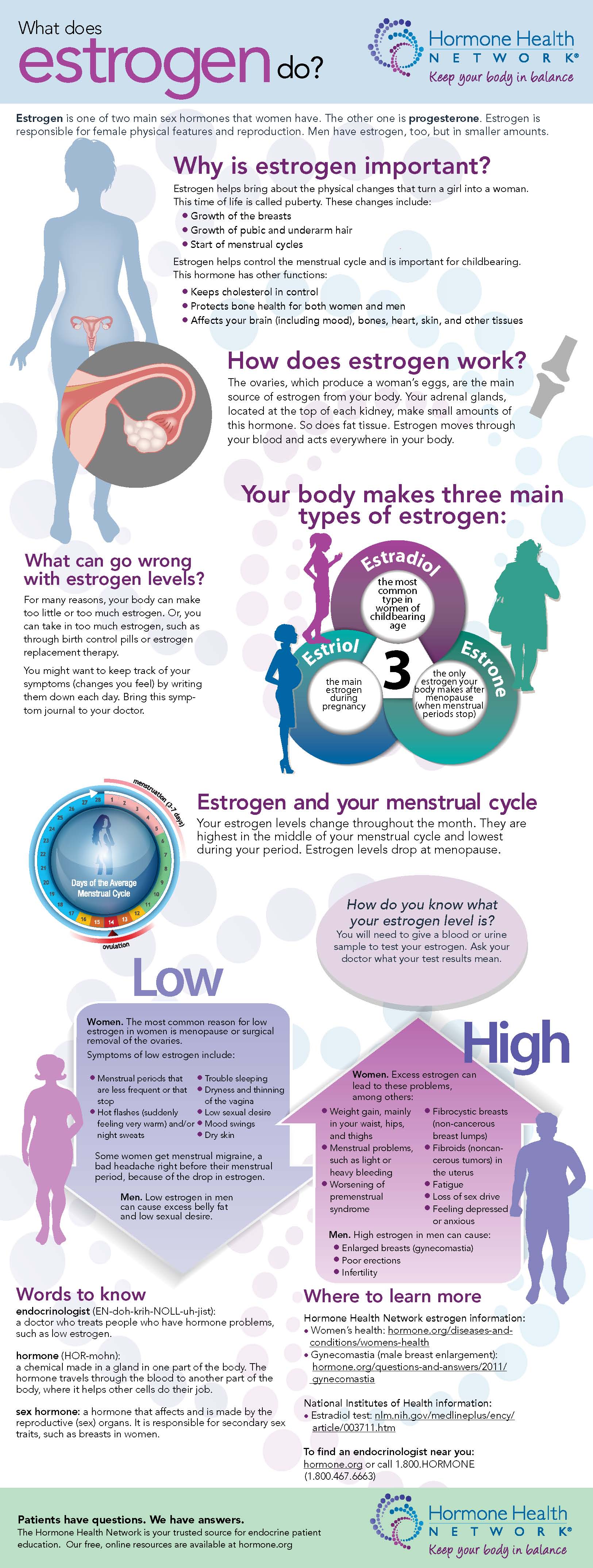
A few months ago, the Endocrine Society sent me an infographic that does a great job distilling this topic down to an understandable level. While I typically stay away from infographics, I like this for a number of reasons, including the fact that it is from a reputable source — the Hormone Health Network.
Read More
Guyside: Getting testy about testosterone
 There’s no doubt that men think about the effects of aging on their bodies. And if there were, a viewing of ads for hair colouring, hair thickening agents, or erectile dysfunction drugs would quickly convince you. You could be a new man!
There’s no doubt that men think about the effects of aging on their bodies. And if there were, a viewing of ads for hair colouring, hair thickening agents, or erectile dysfunction drugs would quickly convince you. You could be a new man!
And as regular Flashfree readers will know, one of the things that’s been touted as a solution to the woes of the aging male is testosterone replacement therapy.
The basic idea is that men may have a condition that’s referred to as “Low T.” And so a gel, a patch, a tablet or an injection may bring you back to a more energetic, athletic, virile condition. The pitch has been made more and more convincingly, by all accounts: an Australian research team found that the sales of testsosterone treatments went from $150 million in 2001 to $1.8 billion in 2012.
That’s a 1200% increase. The Australian research indicated that the amount of testosterone being prescribed far outstripped the incidence of “male menopause” or andropause. So what’s going on? Oh, I suspect there’s a generous helping of vanity involved here.
But if it were simply a matter of making men feel better about themselves, it would just be a waste of money. A growing body of research evidence is suggesting that treating Low T may increase the risk of cardiac events. The most recent, an article from the open-access journal PLOS ONE, suggests a substantial increase in the risk of myocardial infarction — what we normally refer to as a heart attack — with the use of testosterone, for men under and over 65 years of age.
I’m sure there are men with diagnostic criteria that would make testosterone therapy an appropriate choice, with a careful calculation of the risks and benefits. But if my hair’s getting a little thin, if I’m not feeling as “macho” as I once was — do I really want to be using a hormone supplement that could put me at risk of a heart attack?
It’s very easy to succumb to marketing-based pitches that appeal to what we think we need as men. But it’s important for us to not jump at those pitches without thinking about the risks and the benefits carefully.
There was a rush to use estrogen and progesterone to help women with symptoms of menopause several years ago, and then a panic when those therapies were associated with increased cardiac symptoms.
I’m no doctor, and I’m certainly not saying that nobody should be using hormones in this way. But I do think that we should think through ALL of our medical decisions and ensure we’re taking the risks seriously.
(photo: CC-licenced image by Flickr user Ed Schipul)
Read MoreNewsflash: So, estrogen is safe?
 If you’ve been following this blog for any period of time, you know that I’ve consistently shared data that demonstrate the hormones, particularly combination hormone replacement therapy (HRT) can be dangerous, depending on age, time since menopause and other concomitant health issues. Yet, the medical community continues to beat the dead horse of trying to prove the hormone replacement in any form has a role in women’s health. And because I have promised to share the facts, regardless of whether or not I have questions about the motivation underlying their derivation, I am writing this post.
If you’ve been following this blog for any period of time, you know that I’ve consistently shared data that demonstrate the hormones, particularly combination hormone replacement therapy (HRT) can be dangerous, depending on age, time since menopause and other concomitant health issues. Yet, the medical community continues to beat the dead horse of trying to prove the hormone replacement in any form has a role in women’s health. And because I have promised to share the facts, regardless of whether or not I have questions about the motivation underlying their derivation, I am writing this post.
According to research appearing in the July 28 online issue of the American Journal of Public Health, estrogen actually prevents deaths among women who have had hysterectomies. By the way, that’s estrogen ALONE, not estrogen plus progestin, and that is a critical distinction.
Onto the findings. When researchers took another gander at the Women’s Health Initiative data, they sought to determine how the rate of excess mortality among women who took placebo versus those who took estrogen over the course of the landmark study actually translated into premature deaths that might have been preventable. And what they found is pretty shocking:
- The researchers looked at deaths in women who had undergone hysterectomy and still had an ovary intact compared with those who did not have any ovaries (note that sightly more than half — 54% — of women have both ovaries removed at the time of hysterectomy)
- They also examined the use of oral estrogen among the 50 to 59 year old set between the years 2001 and 2004, noting a decline by as much as 60% (largely the result of the the findings of the Women’s Health Initiative) and a relative decline by as much as 71% by the year 2009.
- In composite, they were able to calculate that between 2002 and 2011, a least 18,601 excess deaths occurred and as many as 91,61o excess deaths occurred among women who had had hysterectomies and chose not to use estrogen. This translates to an actual toll attributed to the decision of 40,292 to 48,835 deaths.
The researchers say that estrogen therapy alone reduces mortality mainly by reducing the number of heart disease-related deaths; notably early surgical menopause and complete removal of the ovaries boost the risk for coronary heart disease. Estrogen prevents the development of atherosclerosis and helps maintain normal blood flow.
It’s important to remember that these findings do not apply to women younger than age 50 or older than age 59. Moreover, they also fail to consider other reasons for the increase in heart disease among women as their estrogen declines, such as a surge in cholesterol. And, despite the improved odds against dying from heart disease, these data also ignore other health issues associated with estrogen alone, such as incontinence, hip fracture and of course, breast cancer among certain subsets of women. Hence, again, I am forced to ask the question why researchers continue to beat this horse to death when the deaths prevented may carry the cost of other issues?
I don’t believe that this is anything that will be resolved any time soon. And, as I have written previously we’re drowning in politics, medicine and industry. And it’s difficult to discern truth from fiction, data from data, risk from benefit. Ongoing analyses will eventually reveal what’s what. Meanwhile, read the library of HRT posts on Flashfree. Talk to your physician. Avoid hasty decisions. And consider alternatives. If the medical community can’t agree, perhaps it’s time to put down the gauntlet and wait out the firestorm.
The choice is yours’. Which side are you willing to err on?
Read MoreWednesday Bubble: U.S. Preventive Services Task Force Recommends Against Use of Hormone Therapy for Chronic Disease Prevention
I just can’t help myself. It’s Monday. But this news item calls for a Wednesday Bubble. And yet another nail in the HRT coffin.
The U.S. Preventive Services Task Force (USPSTF) issued an update to its 2005 statement on hormonal therapy late this afternoon. It reads:
“The U.S. Preventive Services Task Force (USPSTF) recommends against the use of of combined estrogen and progestin for the prevention of chronic conditions in postmenopausal women” (evidence grade D – There is moderate or high certainty that the service has no net benefit or that the harms outweigh the benefits).
“The USPTF recommends against the use of of estrogen for the prevention of chronic conditions in postmenopausal women who have had a hysterectomy (D recommendation).
Wondering what this means?
The USPTF recommendations are clear that they refer to the use of HRT and hormone therapy for the purpose of reducing a woman’s risk of developing certain chronic diseases, such as heart disease or dementia and not for the purpose of treating considering hormone therapy for menopausal symptoms such as hot flashes or vaginal dryness/atrophy. However, they are also clear about the data that explores the use of hormone therapy for chronic diseases, noting that while combined HRT has been shown to decrease the risk for fractures, this decline is accompanied by an increase in the risk for serious events that include:
- stroke
- invasive breast cancer
- dementia
- gallbladder disease
- blood clots in the veins or lungs
Additionally, they report that data do not demonstrate a decrease in heart disease and even show an increased likelihood — 1.22 times the norm — for some type of heart event.
For estrogen alone, they again note the benefits in terms of fracture reductions and even a small decline in risk of developing or dying from invasive breast cancer (e.g. 8 fewer cases or 2 fewer deaths per 10,000 person years). However, estrogen-alone has also been associated with “important harms” including:
- stroke
- blood clots in the veins
- gallbladder disease
Like combined hormone therapy, estrogen alone does not reduce the risk for coronary heart disease.
The Task Force also points out that both forms of hormone therapy have been associated with an increased incidence of stress, mixed or urge urinary incontinence after one year.
Mind you, naysayers will say that the average age of women participating in the Women’s Health Initiative were a bit older than the vast majority of women who are transitioning through menopause. To a certain extent, the Task Force agrees, calling for “new research to help better define whether there is a differential balance of benefits and harms based on age at initiation, duration of use and dose or delivery mechanism. Still, they conclude with “high certainty that there is zero to negative net benefit for the use of combined estrogen and progestin therapy for the prevention of chronic conditions and concludes with moderate certainty that there is no net benefit for use of estrogen alone.” Moreover, major health organizations are aligned with the new recommendations. For example, the American Heart Association and American Congress of Obstetricians and Gynecologists recommend against using hormonal therapy to prevent heart disease. The Canadian Task Force on Preventive Health Care and American Academy of Family Physicians are totally aligned with the USPSTF in terms of the use of hormonal therapy to prevent chronic illness in postmenopausal women. Even the North American Menopause Society, a huge proponent of hormone therapy, does not believe that hormones should be used to protect the heart or prevent dementia.
Let’s place the recommendations in context.
By the time most women reach menopause, they are expected to live at least 30 additional years. During this time, they have varied risks for developing chronic diseases, ranging from 30% for coronary heart disease and 21% for stroke to 22% for dementia and 11% for breast cancer. In an accompanying press release, Associate Professor of Medicine and of Epidemiology and Biostatistics at the University of California, San Francisco , Dr. Kirstin Bibbins-Domingo, says “the Task Force recommends a number of important preventive measures women can take to prevent chronic diseases, including quitting smoking and identifying and treating high blood pressure and high cholesterol. There are also other effective ways that women can reduce their risk of bone fractures, such as weight-bearing exercise and being screened and treated, as appropriate for osteoporosis.”
In other words, speak to your practitioner about evidence-based strategies to maintain good health and prevent disease. In this case, the evidence for HRT in disease prevention efforts during menopause is scant and the risks appear to outweigh the benefits.
Read More
Hormones and sex
About a year ago I wrote several posts cautioning women that use of topical hormone gels or sprays could place both pets and children at risk for early puberty, swelling of vulvas, enlarged mammary glands and even small penises. But what about your partner during sexual intimacy? Does a similar danger exist?
Evidently it does, at least according to data from a very very small study that was published in the Journal of Reproductive Medicine about four years ago. In fact, postmenopausal women who used vaginal estradiol cream (e.g. Estrace) and then had intercourse placed their male partners at risk for a significant increase in estradiol levels in their blood. Moreover, vaginal estradiol cream evidently affected 80% of the men who had intercourse with women using vaginal hormones. On the flip side? Intercourse resulted in lower levels of estradiol in women using the cream. Notably, these changes were minimal but the researchers noted that over time and with long-term exposure, men might start to develop changes associated with feminine hormones such as those seen in small children and pets.
If you are going to use topical or vaginal hormones, be smart about them. Topical hormones should be applied to areas that are not exposed to children or that may be licked by pets, such as the inner thigh. After a certain time period, vaginal estradiol cream can be used one to three times weekly in some women; speak to your practitioner about your treatment and if you can cut back on certain days in order to protect your male partner. An ounce of prevention can protect those you love and may even enhance your sex life!
Read MoreNewsflash! U.S. Preventive Services Task Force Weighs in on HRT
Just like the Energizer bunny. HRT and bad news. When are women and practitioners going to believe the data and stop trying to find the silver lining?
This month’s news is from the U.S. Preventive Services Task Force, who issued a recent update of the evidence for or against the use of hormone replacement for menopausal symptoms; that update appears in the online edition of Annals of Internal Medicine.
Rather than bore you with the details, I’m going to cut to the chase and get to the heart of their findings:
- Estrogen plus progestin or estrogen alone provides significant protection against hip and vertebral fractures that result from osteoporosis and aging.
- Contrary to initial results from the Women’s Health Initiative study, use of estrogen plus progestin significantly increases the risk for invasive breast cancer. Estrogen alone offers some protection against invasive breast cancer.
- Updated analyses also demonstrate that combination HRT also significantly increases risk for stroke, blood clot events, death from lung cancer, gallbladder disease and urinary incontinence.
- Estrogen alone increases the risk for stroke, blood clot events, gallbladder disease and urinary incontinence.
One of the primary arguments that proponents of hormone therapy have used consistently is that these data are restricted to women who are older and are not applicable to women who are perimenopausal or in the earliest stages of menopause. And yet, a variety of medical organizations caution against using HRT as a chronic disease prevention strategy, including the Canadian Task Force on Preventive Health Care, American Heart Association and American College of Obstetricians and Gynecologists.
Even the FDA posits that if you are going to use hormone replacement, you should use it in the short-term and only for ameliorating menopausal symptoms or preventing bone loss. And yet, if you read through four years of Flashfree or click on the tag cloud, you’ll find a number of alternative strategies to offer relief without the slippery risk slope.
What more can I say? Be informed so that you can make informed decisions. If a few less hot flashes or night sweats in the short term means a potential road of illness in the long-term, the benefit-risk ratio may not be worth it. Then again? Only you can decide.
Read More