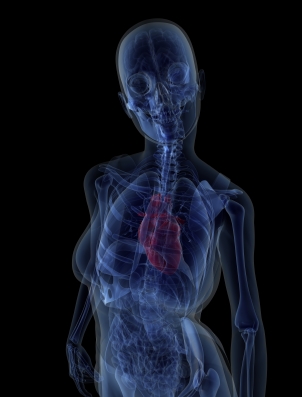
Heart disease and bone health. Is there a link?
It’s crazy, right? Not only do we have to worry about an increased risk of developing heart disease and osteoporosis and related fractures as we age, but it now appears that the two may be linked. In fact, in a study that will be published early next year in the journal Bone, researcher have found that an increased risk of fracture risk is associated with an increased risk of heart and related illnesses.
The findings, which are based on scientifically verified fracture and cardiovascular measures, show that among more than 300 healthy perimenopausal and post menopausal women who had the greatest likelihood for developing heart disease were 5.4 tines more likely to have a higher risk of a major fracture due to osteoporosis and bone loss, and 3 times more likely to have a higher hip fracture risk than women in the lower heart disease risk categories. This likelihood remained even after adjusting for factors such as years since beginning menopause, BMI, smoking and alcohol use, history of HRT use and level of physical activity.
The researchers acknowledge that although aging has been associated with both of these diseases, the link between the two cannot be explained by age alone.Indeed, other studies have shown that women with high cholesterol levels and other blood fat issues have lower bone mineral density measure. While more work needs to be done, the implication is clear: some of the many issues we potentially face as we age may be linked, especially among women. The message is pretty clear as well: take care of your bones and your heart benefits and visa versa.
Read MoreAn apple a day…
Do you recall last year’s post on the beneficial effects of dried plums (aka prunes) on bone health? Well, it appears that dried plums are not the only functional fruit in town. In fact, eating just 2.6 ounces of dried apple daily may protect your heart after menopause.
In this study (published in the August issue of the Journal of The Academy of Nutrition and Dietetics) researchers asked 160 postmenopausal women to eat dried apple or the nutritional equivalent (in terms of calories, fat, carbs, fiber and protein) of dried plums — 3.5 oz — daily for a year. At various time points during the study, levels of blood fats and cholesterol, physical activity and diet were measured. However, the women were asked to avoid taking any steps towards further altering their diets. None of them were on hormone therapy or taking cholesterol lowering drugs during and at least three months before the trial.
The findings are striking. Not only did women who ate dried apple drop 3 pounds, but by three months, their total cholesterol levels had decreased by 9% and LDL-cholesterol levels by 16%. By 6 months, these improvements increased to 13% and 24%, respectively. Moreover, the ratio of HDL to LDL cholesterol improved and C-reactive protein (a protein in the blood that responds to increases in inflammation) declined by 32 %. Women who ate dried plums also experienced improvements in these markers but not to the same dramatic extent.
Eating apples have been linked to improvements in body weight, blood fats, inflammation and other factors that contribute to heart disease. When dried, they are rich sources of soluble fiber and pectin and even suppress food intake, thereby leading to weight loss. Apples are also an excellent source of polyphenols — antioxidant-rich chemicals — that have also been shown to lowering heart disease risk.
Heart disease is a major problem in women and especially after menopause. There are numerous posts within Flashfree that explain the numerous factors that contribute to risk, including elevated cholesterol levels and weight gain. Dried apples represent a cost-saving alternative to statin drugs, which are frequently used to treated high cholesterol while also increasing the risk for muscle weakness and liver damage. Moreover, statins contribute to more than 3% of the total costs of heart disease in the U.S., which is pretty striking.
An apple a day? Sound advice, indeed!
Read More
Under pressure: still drinking the HRT kool-aid?
 Proponents of hormone replacement therapy (HRT) want you to believe that the only negative analyses that are being published are the ones that examine data from the Women’s Health Initiative study. Guess what? That is not true. In fact, there is an evolving body of literature looking at other studies that are coming to similar conclusions: HRT may be a panacea for hot flashes, night sweats and mood swings. But when it comes to cancer and heart disease, you’ve got to be vigilant and aware of your risks. And yet, women continue to be ‘under pressure’ to look the other way, embrace the ‘same as it ever was’ and sift through the facts and fallacies.
Proponents of hormone replacement therapy (HRT) want you to believe that the only negative analyses that are being published are the ones that examine data from the Women’s Health Initiative study. Guess what? That is not true. In fact, there is an evolving body of literature looking at other studies that are coming to similar conclusions: HRT may be a panacea for hot flashes, night sweats and mood swings. But when it comes to cancer and heart disease, you’ve got to be vigilant and aware of your risks. And yet, women continue to be ‘under pressure’ to look the other way, embrace the ‘same as it ever was’ and sift through the facts and fallacies.
Nowhere is the confusion greater than with heart disease. Some data show that long-term HRT protects against heart disease while others suggest that HRT does not.
So does it or doesn’t it?
According to study findings published this month in PLOS ONE, it does not. In fact, the longer you use HRT, the greater your risk of developing high blood pressure, a major, proven factor in heart disease. Here’s what you need to know about this latest information:
- Researchers examined information collected on over 43,000 Australian women who were part of a large-scale study on aging. The women were 45 and older, postmenopausal, had an intact uterus and had not been diagnosed with high blood pressure prior to entering menopause.
- Factors that might influence high blood pressure risk, such as obesity, smoking or lack of physical activity were also examined. On average, the women in the study who used HRT reported having sufficient levels of physical activity, were past (but not current) smokers, drank alcohol and had a healthy body-mass index.
- In the study, the average age that women entered menopause and had ever used HRT was 48 years and most were about 52 years old when they started hormone replacement. Comparatively, women who used HRT developed high blood pressure by age 58.
- The findings showed that younger women (<55 to 61 years) who used HRT had 1.5 times the odds of developing high blood pressure than women who did not. The risk dropped slightly as women got older (between the ages of 62 and 70, HRT users had 1.2 times greater odds of high blood pressure).
- The longer that HRT was used, the greater the odds of developing high blood pressure, with highest risk among women who had used hormone replacement for 6 to 10 years or more. Again, as women in the study age, this risk appeared to decline.
One of the biggest criticisms of the Women’s Health Initiative was that it looked at an older group of women who were not representative of the average age that menopause starts. Here, the data show that in younger women, the odds of HRT being associated with high blood pressure are significant regardless of other potential confounding lifestyle factors. The investigators say that women should be prescribed HRT for the shortest time as possible and that they should be closely monitored for blood pressure before, during and after they stop hormones. Further, they state that “high blood pressure should be conveyed as a health risk for people considering MHT (menopausal hormonal therapy) use.” They also add that these recommendations are aligned with current recommendations for hormone use by the US Food & Drug Administration.
Are you still drinking the HRT kool-aid? You may want to switch beverages, especially if you care about your heart.
Read MoreHave a heart: low carb, high protein diets
This post will not be very popular amongst some people. And I apologize in advance for that. But I only share information that you may find useful; it’s up to you to decide how to use it.
Lately, there’s been a craze to consume diets high in protein and low in carbs in order to stave off weight and theoretically, certain diseases. But what if a diet out of balance is placing your heart at risk? That’s exactly what researchers are reporting in a large study of almost 44,000 Swedish women that was published this week in the open access British Medical Journal. You can find that study here. Mind you, the researchers caution that the findings don’t address whether or not there are benefits to eating such a diet in the short term. But this is what they do show:
- After examining questionnaires collected over a 15+ year period in this group of relatively young women (ages 30 to 49), they observed 1,270 heart events, including heart disease, stroke, hemorrhage and peripheral disease of the arteries.
- When they scored the diets based on protein or carb intake (with 1 being ‘very high’ and 10, ‘very low) or a mixed diet (with 2 associated with hi carb/lo protein and 20, every low carb and very high protein) they learned that a 1 point decline in intake of carbohydrates or 1 point increase in protein was associated with a 4% increase in heart events.
- Each 2 point increase in low carb/high protein diets (which is equivalent to a 5 gram increase in daily protein intake and a 20 gram decline in daily carbohydrate intake, was linked to a significant 5% increase in heart events. Moreover, these risks did not differ substantially among women whose protein intake primarily derived from animal or plant origin.
The researchers state that “vegetables, fruits, cereals and legumes, which have been found in several studies to be core components of healthy dietary patterns, are important sources of carbohydrates so reduced intake of these food groups is likely to have adverse effects on cardiovascular health,” adding that “several studies have reported that meat consumption or hight intake of protein from animal sources may increase the risk of cardiovascular disease.”
So, what’s the primary message here? Well, like any other study, nothing is definitive. And yet, we know that heart disease risk naturally increases as women age. Should you continue to ascribe to the low-carb/high-protein craze, you may want to pay extra attention to your heart health. You may look like a million bucks and your insulin levels may be fabulous but your heart may be struggling to keep up. Meanwhile? Concentrate on low fat animal proteins and try to stay with the 80-20 rule if you refuse to change your ways, i.e., 80% protein, 20% carbohydrates. Seriously? Have a heart.
Read MoreWednesday Bubble: Flashes and sweats and your heart
Be still my heart? Not this week. At least not as far as hot flashes and night sweats go. In fact, study findings that will be presented this coming weekend at the Endocrine Society ‘s 94th Annual Meeting suggest that hot flashes and night sweats that many women experience early in their menopause are not related to an increased risk for heart disease.
So what’s the 4-11?
Researchers have previously questioned whether or not timing of symptoms play a role in a woman’s increased risk for heart disease during menopause. They’ve found that experiencing symptoms only around the time menopause begins may actually reduce the risk for heart disease, or the risk of stroke, heart attack or death (compared with women who experience symptoms later). (If you’d like more about heart disease, aging and menopause, an archive of posts can be found here). To learn more, they have now analyzed the presence of markers in the body that have been linked to heart disease risk (e.g. high blood pressure, cholesterol, blood sugar, insulin, and specific blood markers that might indicate inflammation), in almost 60,000 women who were in menopause and had participated in the Women’s Health Initiative Observation Study.
These women were separated into groups, depending on the presence and timing of vasomotor symptoms:
1) No symptoms
2) Symptoms at start of menopause but not at the start of the study
3) Symptoms both at the start of menopause and the start of the study
4) Symptoms at the start of the study but not at the start of menopause
Importantly, women who had symptoms early in their menopause but not late did not appear to have elevated markers that may indicate heart disease risk. In comparison to this group, women whose vasomotor symptoms occurred only late in menopause appeared to have increased risk, mainly due to higher blood pressure and higher white blood cell counts. Those whose symptoms started early and persisted appeared to have higher levels of glucose and insulin, which indicated an increase in the risk for diabetes.
The researchers, who harken from Northwestern University, note that it’s unclear why timing of symptoms may influence heart disease, although the lead investigator, Dr. Emily D. Szmuilowicz has speculated that symptoms that occur long after menopause begin may indicated some sort of blood vessel abnormality. And while she and her colleagues have not suggested a strategy to attenuate this risk, it is clear that due diligence is needed. If your symptoms persist well into your menopause, see your health practitioner and ask him or her to run some tests. More importantly, hindsight is 20-20; be sure to instill lasting heart healthy habits early and maintain them while you age.
Read More
No time like a present: heart disease, metabolic syndrome and weight
Want to give yourself the gift of a lifetime? Aim for a healthy weight before you hit menopause.
We’ve discussed it time and again on Flashfree; weight gain and menopause go hand in hand like a horse and carriage. And with that weight gains comes an increased risk for developing heart disease, diabetes and the dreaded metabolic syndrome. However, researchers from the University of Ottawa are reporting that entering full menopause with a healthy body mass index (BMI) actually confers protection.
In the study (which appeared online a few weeks ago in the journal Menopause), researchers evaluated and observed 102 premenopausal women for body composition and changes in their cardiovascular health profiles. The women, all of whom were between 47 and 55 years of age, did not smoke, had a BMI between 20 and 29 and had had a stable weight for at least 6 months before the study started, were followed for five years. Each year, the researchers gauged if they had entered menopause, measured body composition (i.e. total fat mass, trunk fat mass and total fat free mass), waist size, the degree of abdominal fat and took blood to examine glucose, insulin and blood fat levels.
The study’s lead researcher, Dr. Denis Prud-homme explains that by simply observing the women and not imposing any structured interventions (e.g. diet or exercise) they were able to assess changes within a more naturalistic environment. At the study’s end, they discovered that despite significant increases in fat mass, visceral abdominal fat, blood glucose and cholesterol levels, most of which were the natural result of hormone fluctuations and aging, the women did not appear to have any declines in their heart or metabolic profiles that would indicate an increased risk for disease. Dr. Prud-homme says that a possible explanation might be that “even if the area of visceral fat is increased, it is still under the critical threshold associated with cardio-metabolic deterioration.” In other words, by maintaing a healthy lifestyle and BMI premenopausally, these women were able to change their risk equations once they fully entered menopause.
The bottom line is that the present you give yourself now will last long into your later years. Exercise. Eat right. And pay attention to your health.
No time like the present. For a present. Give yourself one.
Read More