Newsflash! Severe hot flashes? Keep an eye out for bone health!
Heads up! If you experience moderate to severe hot flashes and night sweats, you may be at higher risk for lower bone density and in turn, a higher rate of hip fractures than women without these symptoms. These study findings were published online yesterday in the Journal of Clinical Endocrinology & Metabolism,
A bit of background…researchers prospectively examined data from over 23,000 women participating in the Women’s Health Initiative study who did not use hormones. The goal was to assess the association, if any between vasomotor symptoms, that is, hot flashes and/or night sweats, and bone mineral density. In turn, they collected self-reports of fractures (i.e. hip, spine, non-vertebral) on a semi-annual basis; these were subsequently confirmed by reviewing medical records.
The findings? Over an average of eight years, women who reported moderate to severe hot flashes or night sweats had almost twice the risk for developing a hip fracture over the time period of the study than women who did not, regardless of a younger age or higher body mass index, or other factors such as time since menopause, race/ethnicity or physical activity. And, while additional analyses did slightly reduce this risk, moderate to severe vasomotor symptoms remained a significant risk factor for hip fracture over the study course. Additionally, the findings demonstrate that women with more severe symptoms had lower bone mineral density measures over time in the hip joint and spine.
Although it’s unclear, the researchers note that lower estradiol levels may account for the association between more severe symptoms and lower bone mineral density (as, data have shown that women with higher estradiol levels during menopause tend to have lower rates of bone loss). Regardless, having more severe flashes and sweats should raise a few red flags for women and their practitioners and prompt greater attention to lifestyle strategies for preserving bone mineral density. This topic has been covered thoroughly on Flashfree, and strategiest include diet, weight-bearing exercise and adequate sun exposure.
Read More
Guyside: Dealing with aging parents, guyside style.

As parents age, we have to move from being “their child” to mutual independence to their dependence on us. It’s not always easy.
One of the things about getting to this age (in my case, 47) is that you get the odd experience of parenting your parents.
I was about the last child in my generation. With both parents near the end of large families, I have a ton of cousins, many of whom are well into retirement by now. And as a late child (born to 41-year-olds), my mom (and my dad, until his death in 2012) is well into seniorhood.
It’s probably no surprise that the dynamics change when your parents age. As a child, we strive for independence from our parents. That lasts for some time and then, like a wave collapsing in on itself and running back into the ocean, dependence begins to reach back out from your parents to you.
Things that were easily done for years become more difficult. It becomes more challenging for the senior citizen to take on some of the frustrations of daily living. And if physical illnesses encroach, as they almost certainly will, that process can accelerate more and more as time goes on.
So here, from my own experience and with the help of some references I’ve found, are some tips for dealing with aging parents:
- Find ways to detach emotionally just a bit. It’s difficult to hear a parent in emotional or health difficulty. But if your emotions take over, it’s going to be difficult to truly help them. Create an outlet for your emotions, but then work on logic.
- Sometimes just listening is enough. As a guy, I know only too well I can jump to SOLVING THE PROBLEM. But sometimes, your parent won’t want a solution; they’ll want a set of ears.
- Talk to your parent or parents about power of attorney. There are times at which you may need to intercede. It’s easier to do that if you have arranged things in advance.
- Support anything your parents are interested in doing that will help their physical, emotional, or mental health. Got a 97-year-old (like my aunt) who loves to swim? Make sure he or she gets to the pool. Is someone a bridge player? Find them a club. Often, seniors lose friends and family members as they age, so new social links are important.
- Build relationships with their health care providers. As seniors age, it’s more likely they’ll have serious health concerns crop up. And seniors are more likely to have a more deferential attitude toward doctors and medical professionals than younger people. So it’s important that you be able to play a role in their health care. This doesn’t mean taking over; it can mean being a trusted resource, an advocate, or maybe just a drive to an appointment.
Wednesday Bubble: When it comes to bone health, D is for “don’t bother”
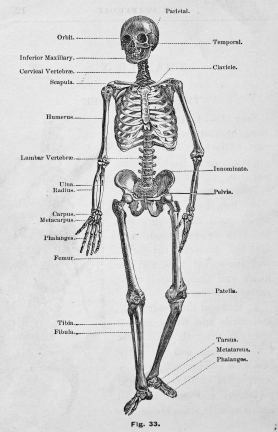
Conventional wisdom suggests that combining calcium with vitamin D improves calcium absorption, and therefore may help prevent fractures resulting from bone loss and the body’s inability to replace bone. Notably, in younger people, the body works efficiently to replace bone after it breaks it down. However, after the age of 30, women begin lose bone mass and as I’ve written time and again in Flashfree, by the time we hit menopause, this process speeds ups, resulting in osteopenia and of course, osteoporosis.
And yet, researchers are now saying that they’ve confirmed that while calcium supplementation (1,200 mg daily) may reduce bone turnover and by default, improve overall bone health, adding vitamin D offers no additional advantage unless a woman has an existing vitamin D deficiency. In this recent study of 159 menopausal women, they compared vitamin D and calcium to calcium alone to vitamin D alone to placebo. They then measured a marker of bone turnover in the blood — PTH, or parathyroid hormone — over a period of six months.
Not surprisingly, they found that when they compared the women taking daily calcium to those who obtained calcium naturally in their diet, calcium was a clear winner, resulting in a significant reduction in bone turnover. However, when vitamin D was added to daily calcium, it did not seem to add any benefit (although it also did no harm).
No harm, no foul?
Not quite. The researchers say that too much calcium is too much of a good thing and that calcium balance is critical. The addition of vitamin D may lead to a condition called hypercalciuria — excessive calcium in the blood — which over time, can impair kidneys. The best practice is a cautious one; consult your practitioner to learn what your calcium levels are and proceed from there. If s/he recommends supplementing natural dietary intake of calcium with supplements, then you are good to go. However, when it comes to D and bone health? Maybe don’t!
In the interim, if you are interested in learning more about calcium do’s and don’ts, the archives hold a wealth of information. Check these posts out!
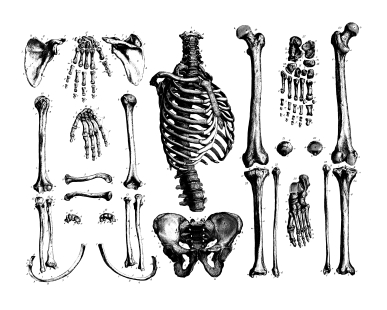
Read MoreOh dem bones! Time to cut your losses.
 Remember the ‘Capture the Fracture’ post from a few weeks back? In it, I reported that the International Osteoporosis Foundation is urging women and men alike to receive screening for bone loss, especially if they had some sort of fracture in their early years. Ironically, over the weekend, a close friend shared that she had been told that she has osteopenia, i.e. low bone mineral density, and it started me wondering how many of my readers have actually gone to their practitioners for a baseline? Me? I am guilty as charged; in fact, because of an absolutely crazy work schedule for most of this year, I’m very much behind on all my health visits.
Remember the ‘Capture the Fracture’ post from a few weeks back? In it, I reported that the International Osteoporosis Foundation is urging women and men alike to receive screening for bone loss, especially if they had some sort of fracture in their early years. Ironically, over the weekend, a close friend shared that she had been told that she has osteopenia, i.e. low bone mineral density, and it started me wondering how many of my readers have actually gone to their practitioners for a baseline? Me? I am guilty as charged; in fact, because of an absolutely crazy work schedule for most of this year, I’m very much behind on all my health visits.
So, back to osteoporosis, osteopenia and fragility fractures. I imagine that many of you are growing tired of reading about these topics on Flashfree but I can’t help myself; they’re vitally important.
According to the National Osteoporosis Foundation, by 2020 — a mere seven years from now — more than half of Americans over the age of 50 are expected to have low bone density or develop osteoporosis. Data also suggest that the risk of hip fracture in women is greater than the risk of all female cancers combined. What’s more, women who experience a hip fracture in their later years have almost a 3-fold risk of dying in the three months that follow.
Are you paying attention yet? You should be, because as I’ve written time and again,within the first 10 years of the onset of menopause, women lose up to 50% of their spongy, or trabecular bone (the network that makes up most of bone structure) and up to 30% of their cortical bone (the outer shell).
However, it’s not just hormones at play. In the latest issue of the International Journal of Medical Engineering and Informatics, Portugese researchers are reporting that several factors appear to be associated with an increased fracture risk in menopausal women with and without a history of fracture, including age over 65, lower bone mineral density (BMD), a sedentary lifestyle, and eating or drinking caffeine-containing foods. In population of 127 women, almost 41% had osteopenia and roughly 20%, osteoporosis. Less than 40% had normal bone mineral density values.
However, these factors are not the only variables that you should be thinking about. Research shows that many medications can contribute to bone loss. They include:
- Aluminum-containing antacids
- Antidepressants (SSRIs), such as Lexapro®, Prozac® and Zoloft®
- Gonadotropin releasing hormone (GnRH) such as Lupron® and Zoladex®
- Heparin
- Lithium
- Depo-Provera®
- Methotrexate
- Proton pump inhibitors (PPIs) such as Nexium®, Prevacid® and Prilosec®
- Steroids such as cortisone and prednisone
- Tamoxifen® (premenopausal use)
- Type 2 diabetes medications (Actos® and Avandia®)
- Thyroid hormones in excess
And, a small case study analysis has shown that if you are a woman who has had estrogen receptor positive breast cancer and previously treated with aromatase inhibitors (e.g. Arimidex, Femura), you have a 27% increase for the risk of bone loss and a 21% risk for a hip fracture at an earlier age. Additionally, these events can occur at a higher bone mineral density level than postmenopausal women who have not had chemotherapy.
Short of starting medical therapy with bisphosphonates (which have a rash of problems associated with their use), what can you do? Clearly, a great place to start is with regular weight-bearing exercise and insuring that your diet contains adequate amounts of calcium and vitamin D, although we know that some of amount of bone loss is inevitable as we age. However, before you become frustrated, there are a few lesser known steps that have clinical evidence behind them:
- Eat prunes. Researchers say that as little as 6 to 10 a day can help boost BMD and reduce rates of bone resorption.
- Incorporate onions into your diet. Onions are another type of functional foods that have been shown to improve bone density.
- Eat more sea fish. Data have shown that who make sea fish (not shellfish or freshwater fish) at least 16% of their daily protein intake have greater BMD.
- Talk to your practitioner about taking the lowest effective dose of the medications listed above.
- Drink moderately. One or two alcoholic drinks a day may be protective. More? Not only does your liver hate you but your bones are at risk too.
There’s bad to the bone. And then, bad to the bone. Time to cut your losses, literally…
Read More
Capture the fracture
Sounds like a new reality show for the over 50 set right? But it’s pretty serious.
A new report from the International Osteoporosis Foundation (IOF) demonstrates that one in two women over the age of 50 are at risk for fragility fractures that may be related to bone loss and not only trauma. In other words, broken hip bones, or bones in the wrist, arm or their vertebrae — usually resulting from a fall — may be a signal that something else is also at play. Moreover, the IOF reports that approximately 80% of both men and women who are treated at clinics or hospitals falling a fracture are not receiving screening for osteoporosis, osteopenia (low bone mineral density) and associated risk for future fractures.
So, why does this matter?
Well, according to IOF statistics, half of people who ultimately end up with a fractured hip in old age had a fragility fracture when they were younger. Moreover, 1/6th of menopausal women have had some sort of fragility fracture in their lives. Considering that women in particular lose up to 50% of their spongy, or trabecular bone (the network that makes up most of bone structure) and up to 30% of their cortical bone (the outer shell) within the first 10 years of the onset of menopause, and the body is creating a perfect storm. According to the IOF, up to a quarter of hip fractures can be prevented by early diagnosis and appropriate osteoporosis testing and follow up treatment.
Mind you, the treatments for osteoporosis are controversial. As I’ve written previously, the most popular drugs for osteoporosis — bisphosphonates — may be risky after about 5 years of use and even increase fracture risk in some women. However, there are important non-pharmacologic steps that can be taken to counterbalance risk, such as:
- Weight bearing exercise
- Insuring that you don’t sit too long at any given time while at work (women who sit for more than 9 hours a day have a 50% increased risk of hip fracture)
- Strengthening back muscles, which can help prevent vertebral fractures
- Insuring that adequate amounts of low-fat dairy, tofu and certain green vegetables are included in your daily diet. Note that some plant foods contain substances that can lower amounts of available calcium to the body, e.g. oxylates in spinach and rhubarb or phytates in dried beans, so you want to be sure to counter that with vegetables like broccoli, kale and bok choy, which are low in these substances.
Even if you eat a proper diet and exercise daily, you are still at risk of bone loss and fracture – it’s a natural result of aging and waning estrogen. However, if you are fifty or older and suffer a fracture, heck even if you are slightly younger, request a screening for bone loss and osteoporosis. The IOF says that most clinicians don’t follow this path — possibly due to cost concerns, time or even where the responsibility for care even lies. The latter is particularly important and is much like the ‘Bermuda Triangle,” where experts say that patients can disappear into a maze of “orthopedists, primary care physicians and osteoporosis experts” only never to be seen again (until they break a hip).
As always, information is power and the first point of care is truly you. Want to stay standing well into old age? Capture the fracture now.
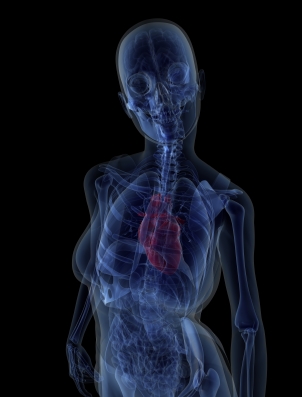
Read MoreHeart disease and bone health. Is there a link?
It’s crazy, right? Not only do we have to worry about an increased risk of developing heart disease and osteoporosis and related fractures as we age, but it now appears that the two may be linked. In fact, in a study that will be published early next year in the journal Bone, researcher have found that an increased risk of fracture risk is associated with an increased risk of heart and related illnesses.
The findings, which are based on scientifically verified fracture and cardiovascular measures, show that among more than 300 healthy perimenopausal and post menopausal women who had the greatest likelihood for developing heart disease were 5.4 tines more likely to have a higher risk of a major fracture due to osteoporosis and bone loss, and 3 times more likely to have a higher hip fracture risk than women in the lower heart disease risk categories. This likelihood remained even after adjusting for factors such as years since beginning menopause, BMI, smoking and alcohol use, history of HRT use and level of physical activity.
The researchers acknowledge that although aging has been associated with both of these diseases, the link between the two cannot be explained by age alone.Indeed, other studies have shown that women with high cholesterol levels and other blood fat issues have lower bone mineral density measure. While more work needs to be done, the implication is clear: some of the many issues we potentially face as we age may be linked, especially among women. The message is pretty clear as well: take care of your bones and your heart benefits and visa versa.
Read More