Wednesday Bubble: Your bones, your health. The lowdown on bisphosphonates
For decades, physicians have been prescribing a class of medications known as bisphosphonates (e.g. Fosamax, Actonel, Boniva) to preserve bone health in menopausal women and prevent fractures in both men and women with osteoporosis at high-risk for them). Bisphosphonates are often offered as an alternative to hormone replacement therapy or HRT.
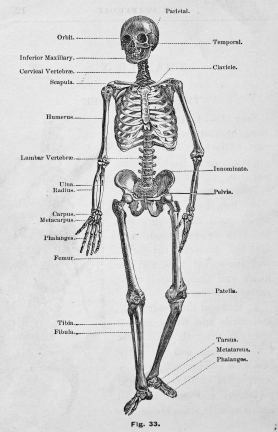
Studies have shown that after age 35, women (and men) start to lose their bone density at a rate of 0.3% to 0.5% a year. However, as estrogen levels decline through menopause, the rate of bone density loss accelerates. In fact, during the first five years after menopause, women can experience as much as a 30% loss of bone density. What’s more, experts estimate that by the time a woman reaches the age of 50, she has a 40% risk of suffering a fracture due to osteoporosis for the rest of her lifetime.
If you consider these statistics, it seems that using bisphosphonates is a good thing, right?
Well, not so fast. Earlier this year, I wrote a post highlighting reports of jaw bones collapsing among women taking bisphosphonates over a certain period of time. Included within the information were tips from the American Dental Association for protecting your jaw before any major dental procedures. This week, I want to add another facet to the bisphosphonate story, one that is definitely worth considering when weighing the benefits and risks of these drugs:
It is possible that use of oral bisphosphonates may increase the risk for developing cancer of the esophagus by as much as two-fold.
Here’s what you need to know:
- In this particular study, researchers compared over 15,000 men and women who had been diagnosed with esophageal, gastric or colon cancer over the age of 40 to five healthy individuals with similar characteristics. All study participants had been prescribed bisphosphonates at least once, with some receiving more than 10 prescriptions, which would imply that they used the drugs over time (over the 7-1/2 year period of times examined, a majority used bisphosphonates for at three years or more).
- Use of bisphosphonates over three years and having received at least 10 prescriptions was linked to a significant increase in cancer of the esophagus but not gastric or colon cancer. People who used bisphosphonates for five years or more had twice the risk compared to those who did not. Note that these rates of cancer held regardless of the exact agent used.
- An increased cancer risk remained even after actors for esophageal cancer, such as age, smoking, alcohol and body mass intake, were accounted for.
- This increased risk, may be due, at least partly, to drug side effects that affect the esophagus directly, such as irritation and inflammation of the esophagus (i.e. esophagitis).
Now, mind you, esophageal cancer is extremely rare, affecting roughly 16,000 people in the US in 2010. However, death from esophageal cancer, is high and the disease is often fatal. Moreover, esophageal cancer tends to affect three to four times as many men as women, which is why this latest bit of information is as critical for men as it is for women entering menopause.
One important thing to keep in mind when you consider the risk and benefits of bisphosphonate therapy is that this particular study compared actual cases of these three types of cancer to healthy individuals in the population. Sometimes, the information yielded in these studies is not considered as conclusive as studies that are conducted proactively, and not retroactively. Still, this is not the first time that bisphosphonates have been linked to cancer of the esophagus.
Maintaining bone health and strength as we age, particularly as hormones decline, is critical to our health in the later years. It’s important to make the right decisions now, while we are still relatively young. Flashfree has plenty of posts on bone health and osteoporosis, and I encourage you to peruse them. When it comes to your bones, it’s not just about ‘use it or lose it,’ but also, the three P’s:
Protection
Proactive
Prepared
Your bones, your health.
Read MoreWednesday Bubble: bisphosphonates…enough to make your jaw drop
[youtube=http://www.youtube.com/watch?v=ZvCI-gNK_y4]
Are you being treated for osteoporosis? Has your doctor told you about a rare but extremely serious side effect of drugs known as bisphosphonates that causes the jaw bone to collapse?
Osteonecrosis is a disease that occurs when the blood supply to bone is cut off. This results can result in pain, limited range of motion and an eventual collapse of the bone in the affected area. According to the American Dental Association, reports of jaw osteonecrosis among very small numbers of patients taking Fosamax for osteoporosis started to emerge in 2003. At higher risk were cancer patients who were receiving intravenous bisphosphonate therapy as part of their treatment. In the majority of patients, osteonecrosis developed after dental surgery.
As I’ve written previously, osteoporosis and low bone mineral density are well-known issues for menopausal women. Studies have shown that after age 35, women (and men) start to lose their bone density at a rate of 0.3% to 0.5% a year. However, as estrogen levels decline through menopause, the rate of bone density loss accelerates. In fact, during the first five years after menopause, women can experience as much as a 30% loss of bone density. What’s more, experts estimate that by the time a woman reaches the age of 50, she has a 40% risk of suffering a fracture due to osteoporosis for the rest of her lifetime.
Bisphosphonates are frequently prescribed as an alternative to estrogen therapy for preserving bone mass during menopause. Although less than 1% of jaw osteonecrosis have been reported in patients taking oral bisphosphonates, recent research suggests that the majority don’t know about possible side effects. In fact, in this particular study of 71 women and 2 men, 82% said they couldn’t recall or were unsure if their physicians had told them about jaw osteonecrosis.
What you need to know
Taking care of your mouth is essential at any age but particularly during menopause. During the transition, women are especially at risk for altered taste and burning mouth syndrome. Additionally, we are learning that the drugs that we take to prevent loss may actually cause bone death in some women.
The American Dental Association recommends that patients inform their dentist and hygienist that they are taking bisphosphonates to prevent osteoporosis so that extra precaution can be taken before any routine or major dental procedures. if you start to experience the following signs and symptoms while taking bisphosphonates, call your doctor and dentist immediately:
- pain, swelling
- gum or jaw infection
- gums that don’t heal
- loose teeth
- jaw heaviness or numbness
- impaired range of motion
- exposed bone
Undoubtedly, the benefits of bisphosphonate therapy definitely outweigh the risks. Still, it is unclear whether or not bisphosphonates will ultimately prove to be as risky as HRT, as there have also been reports of hip fractures in a very small amount of women taking these drugs for five years or more.
Unfortunately, there are few medicinal alternatives available in the United States, although a new drug Prolia, was approved for treatment of osteoporosis just yesterday. I don’t know much about Prolia, other than it is an agent that has been widely used in treating cancer patients. However, there are some early indications that Prolia might also cause jaw osteonecrosis. Only time will tell.
Meanwhile, I can’t emphasize enough that physical activity and ample calcium and vitamin D intake are essential. The risk of doing nothing now? Enough to make your draw drop…literally.
Read MoreOh dem bones! Time to cut your losses.
 Remember the ‘Capture the Fracture’ post from a few weeks back? In it, I reported that the International Osteoporosis Foundation is urging women and men alike to receive screening for bone loss, especially if they had some sort of fracture in their early years. Ironically, over the weekend, a close friend shared that she had been told that she has osteopenia, i.e. low bone mineral density, and it started me wondering how many of my readers have actually gone to their practitioners for a baseline? Me? I am guilty as charged; in fact, because of an absolutely crazy work schedule for most of this year, I’m very much behind on all my health visits.
Remember the ‘Capture the Fracture’ post from a few weeks back? In it, I reported that the International Osteoporosis Foundation is urging women and men alike to receive screening for bone loss, especially if they had some sort of fracture in their early years. Ironically, over the weekend, a close friend shared that she had been told that she has osteopenia, i.e. low bone mineral density, and it started me wondering how many of my readers have actually gone to their practitioners for a baseline? Me? I am guilty as charged; in fact, because of an absolutely crazy work schedule for most of this year, I’m very much behind on all my health visits.
So, back to osteoporosis, osteopenia and fragility fractures. I imagine that many of you are growing tired of reading about these topics on Flashfree but I can’t help myself; they’re vitally important.
According to the National Osteoporosis Foundation, by 2020 — a mere seven years from now — more than half of Americans over the age of 50 are expected to have low bone density or develop osteoporosis. Data also suggest that the risk of hip fracture in women is greater than the risk of all female cancers combined. What’s more, women who experience a hip fracture in their later years have almost a 3-fold risk of dying in the three months that follow.
Are you paying attention yet? You should be, because as I’ve written time and again,within the first 10 years of the onset of menopause, women lose up to 50% of their spongy, or trabecular bone (the network that makes up most of bone structure) and up to 30% of their cortical bone (the outer shell).
However, it’s not just hormones at play. In the latest issue of the International Journal of Medical Engineering and Informatics, Portugese researchers are reporting that several factors appear to be associated with an increased fracture risk in menopausal women with and without a history of fracture, including age over 65, lower bone mineral density (BMD), a sedentary lifestyle, and eating or drinking caffeine-containing foods. In population of 127 women, almost 41% had osteopenia and roughly 20%, osteoporosis. Less than 40% had normal bone mineral density values.
However, these factors are not the only variables that you should be thinking about. Research shows that many medications can contribute to bone loss. They include:
- Aluminum-containing antacids
- Antidepressants (SSRIs), such as Lexapro®, Prozac® and Zoloft®
- Gonadotropin releasing hormone (GnRH) such as Lupron® and Zoladex®
- Heparin
- Lithium
- Depo-Provera®
- Methotrexate
- Proton pump inhibitors (PPIs) such as Nexium®, Prevacid® and Prilosec®
- Steroids such as cortisone and prednisone
- Tamoxifen® (premenopausal use)
- Type 2 diabetes medications (Actos® and Avandia®)
- Thyroid hormones in excess
And, a small case study analysis has shown that if you are a woman who has had estrogen receptor positive breast cancer and previously treated with aromatase inhibitors (e.g. Arimidex, Femura), you have a 27% increase for the risk of bone loss and a 21% risk for a hip fracture at an earlier age. Additionally, these events can occur at a higher bone mineral density level than postmenopausal women who have not had chemotherapy.
Short of starting medical therapy with bisphosphonates (which have a rash of problems associated with their use), what can you do? Clearly, a great place to start is with regular weight-bearing exercise and insuring that your diet contains adequate amounts of calcium and vitamin D, although we know that some of amount of bone loss is inevitable as we age. However, before you become frustrated, there are a few lesser known steps that have clinical evidence behind them:
- Eat prunes. Researchers say that as little as 6 to 10 a day can help boost BMD and reduce rates of bone resorption.
- Incorporate onions into your diet. Onions are another type of functional foods that have been shown to improve bone density.
- Eat more sea fish. Data have shown that who make sea fish (not shellfish or freshwater fish) at least 16% of their daily protein intake have greater BMD.
- Talk to your practitioner about taking the lowest effective dose of the medications listed above.
- Drink moderately. One or two alcoholic drinks a day may be protective. More? Not only does your liver hate you but your bones are at risk too.
There’s bad to the bone. And then, bad to the bone. Time to cut your losses, literally…
Read More
Capture the fracture
Sounds like a new reality show for the over 50 set right? But it’s pretty serious.
A new report from the International Osteoporosis Foundation (IOF) demonstrates that one in two women over the age of 50 are at risk for fragility fractures that may be related to bone loss and not only trauma. In other words, broken hip bones, or bones in the wrist, arm or their vertebrae — usually resulting from a fall — may be a signal that something else is also at play. Moreover, the IOF reports that approximately 80% of both men and women who are treated at clinics or hospitals falling a fracture are not receiving screening for osteoporosis, osteopenia (low bone mineral density) and associated risk for future fractures.
So, why does this matter?
Well, according to IOF statistics, half of people who ultimately end up with a fractured hip in old age had a fragility fracture when they were younger. Moreover, 1/6th of menopausal women have had some sort of fragility fracture in their lives. Considering that women in particular lose up to 50% of their spongy, or trabecular bone (the network that makes up most of bone structure) and up to 30% of their cortical bone (the outer shell) within the first 10 years of the onset of menopause, and the body is creating a perfect storm. According to the IOF, up to a quarter of hip fractures can be prevented by early diagnosis and appropriate osteoporosis testing and follow up treatment.
Mind you, the treatments for osteoporosis are controversial. As I’ve written previously, the most popular drugs for osteoporosis — bisphosphonates — may be risky after about 5 years of use and even increase fracture risk in some women. However, there are important non-pharmacologic steps that can be taken to counterbalance risk, such as:
- Weight bearing exercise
- Insuring that you don’t sit too long at any given time while at work (women who sit for more than 9 hours a day have a 50% increased risk of hip fracture)
- Strengthening back muscles, which can help prevent vertebral fractures
- Insuring that adequate amounts of low-fat dairy, tofu and certain green vegetables are included in your daily diet. Note that some plant foods contain substances that can lower amounts of available calcium to the body, e.g. oxylates in spinach and rhubarb or phytates in dried beans, so you want to be sure to counter that with vegetables like broccoli, kale and bok choy, which are low in these substances.
Even if you eat a proper diet and exercise daily, you are still at risk of bone loss and fracture – it’s a natural result of aging and waning estrogen. However, if you are fifty or older and suffer a fracture, heck even if you are slightly younger, request a screening for bone loss and osteoporosis. The IOF says that most clinicians don’t follow this path — possibly due to cost concerns, time or even where the responsibility for care even lies. The latter is particularly important and is much like the ‘Bermuda Triangle,” where experts say that patients can disappear into a maze of “orthopedists, primary care physicians and osteoporosis experts” only never to be seen again (until they break a hip).
As always, information is power and the first point of care is truly you. Want to stay standing well into old age? Capture the fracture now.
Read MorePlums…delicious, sweet. And, good for bone health?
[Image: all rights reserved 2012. Used with permission by Tartella. Visit them online at http://www.tartella.com/ and if you love this print as much as I do, you can purchase it in their Etsy store.]
Yowza! I am excited about study findings published in the British Journal of Nutrition linking dried plums (better known as the lowly prune) to improved bone mineral density in menopausal women. If these findings ring true and can be duplicated in larger groups of women, they may have a tremendous impact on the steps we take to preserve our bones as we age — most notably, the ability to avoid bisphosphonates — which have been linked to collapse of jaw bones and even an increase in the fractures they are supposed to protect. Moreover, although calcium supplementation is broadly recommended, there is an indication that it may increase heart disease risk in some women.
However, as one of the investigators note in BJN, study findings consistently show that greater intakes of fruits and vegetables have positive effects on bone resorption (the breakdown of bone), adding prunes among fruits and onions among vegetables, to be the most effective functional foods in terms of their actions on modulating the process by which bones break down and build up again.
In animal studies, prunes were shown to prevent bone loss as well as restore bone mineral density in conditions created to mimic bone loss associated with osteoporosis. In addition to these studies, researchers had also a conducted a short, three-month study in menopausal women in whom bone mass was improved simply by eating around 10 prunes (100 g) daily.
In this latest iteration, the same researchers compared two groups of menopausal women assigned to eat around 100 gm of prunes (~10) or 75 gm dried apples (the equivalent of the prunes in terms of energy, carbohydrates, fats and fiber) daily for a year. All of the women had been in menopause for anywhere from one to 10 years, were not on hormone therapy and were also asked to take 500 mg calcium plus 400 IU vitamin D with their daily dried fruit.
The findings? By the end of one year, women eating prunes had significantly lower levels of several markers for bone turnover compared to their peers who ate dried apple. Conversely, the prune eaters had significantly higher levels of bone mineral density in their ulnas (one of two long bones in the forearm) and spine compared to the other group. The researchers say that this is partly due to the fact that prunes suppress the rate at which bone cells break down bone, which exceeds the rate at which they build it up as we age.
Women in particular lose up to 50% of their spongy, or trabecular bone (the network that makes up most of bone structure) and up to 30% of their cortical bone (the outer shell) within the first 10 years of the onset of menopause. Of the investigators, Professor and chair of Florida State University’s Department of Nutrition, Bahram Arjmandi, suggests that women (and men) interested in maintaining or even improving bone health start eating two to three prunes a day and gradually build to six to 10. Arjmandi says to “do something meaningful and practical beforehand, ” and “don’t wait until you get a fracture or are diagnosed with osteoporosis” and need medication.
Sure, prunes get a bad rap. But aren’t ‘bad’ bones even worse? Truly, prunes can be ‘as delicious and sweet’ as plums. The writing on the wall suggests that you don’t wait until it’s too late.
Read More