Hot flashes, acupuncture and Traditional Chinese Medicine
Acupuncture continues to top the list of ‘go to’ alternatives for hot flashes. And despite confusion, researchers remain focused on trying to explain (and perhaps overcome) conflicting study findings. That, my dear readers, is a very good thing, as this non-invasive, gentle treatment modality, while not the end all to be all, may one day become as accepted among Western practitioners as pharmaceutical agents are.
The goal of Traditional Chinese Medicine (TCM) and acupuncture as they relate to menopausal symptoms like flashes is to reinforce the kidneys, which according to TCM philosophy, result due to a decline in kidney yin and yang (think: out of balance). As I wrote a few years ago:
TCM and other similar philosophies emphasizes various body systems that together, form a network or grid connected by a meridien, if you will, as well as the relationship of the body to its social and natural environment. Its primary focus on maintaining health and enhancing the body’s ability to fight off disease. TCM will not focus, for example, on treating specific pathogens but rather, on addressing non-specific factors that create disturbances or imbalances within a certain network. TCM also examines how these imbalances may occur in unique parts of a specific system, such as the heart and blood vessels and small intestine (all of which are part of the heart system) and how they change over time. Western medicine, on the other hand, focuses primarily on treating morbidities, or symptoms related to various conditions and diseases. You can read more rabout TCM in this post from September, 2010.
In TCM, menopausal symptoms are believed to be related to a decline in yin or yang in the kidneys. One of the oldest prescriptions in TCM to reinforce kidney energy is known as ‘Qing E Fang’ (QEF) and the first record of its use dates back to the year 960. The preparation is a combination of four key ingredients that are mediated through estrogen receptors and expression, hence, its potential usefulness in menopause. (These ingredients, in case you are interested, are Cortex Eucommiae (whose bark and leaf have an antioxidant effect) Fructus Psoraleae (commonly used for bone health and to treat estrogen associated diseases), Semen Juglandis and Rhizoma Garlic.)
From a Western perspective, there is evidence (albeit preliminary) that suggests that acupuncture actually inhibits the thermoregulatory action of the hypothalmic-pituitary gland that works to create a hot flash. (You can read more about how a hot flash comes about here.) And when study trials are designed with TCM and acupuncture philosophy in mind, they tend to yield positive results – such as a small study that appears online in Menopause journal.
This time, researchers took four groups of women who experienced 20 or more hot flashes a week and assigned them to one of four groups: real acupuncture, sham acupuncture (needles inserted superficially), a 14 herb chinese formulation known as Zhi Mu 14 or a placebo version of the same. Women in all four groups were exposed to licensed practitioners and received TCM diagnoses. An important distinction in this research was that not only did the researchers predetermine 8 standard sites for needle insertion, BUT they also allowed the clinician to use an additional, individual points. In the sham acupuncture group, the acupuncture points corresponded to those used regularly in large clinical trials. Women using the Zhi Mu or the placebo took three capsules daily. And, all women maintained a hot flash and menopause symptom diary.
The findings are intriguing. While Zhi Mu did not appear to have much impact on hot flashes, acupuncture did, resulting in significant improvements in both hot flash frequency and severity as well as in other symptoms. Over the long term, acupuncture also appeared to attenuate bladder and sexual problems as well as joint and muscle aches and pains. Moreover, the findings also suggested that real acupuncture is superior to sham acupuncture in reducing severity and frequency of menopausal symptoms, much more so than other clinical trials. Importantly, the researchers believe that their results, albeit preliminary, are due to standardized plus individualized treatment performed by highly experienced acupuncturists.
Where are the holes? Well, this was a small group of women and Zhi Mu doses were not modified according to individual needs (as they might have been in the real world). They also did not test liver values at the end of the study (evidently Zhi Mu has been linked to liver toxicity in some women) so safety of this particular preparation was not properly assessed. Still, scientific jargon aside, this is what you need to take away from this information:
A very small study that was designed by Western practitioners within the parameters of TCM philosophies once again demonstrated the beneficial effect of acupuncture on hot flashes in particular. When acupuncture is conducted appropriately and by a highly skilled practitioner, positive benefits may be realized.
Before we jump to any future conclusions, it’s time to revisit and consider the value of alternatives for menopausal symptoms. Sometimes a spade simply is not a spade and there is more than meets the eye when you start digging through the details.
Read More
Wednesday Bubble: The Glass Ceiling is a Myth
Earlier this week. Fox Business ran a piece claiming that the gender pay gap was nothing more than a myth. Some of the more interesting conclusions suggested that there are fewer women in select fields was because they choose to work in industries that pay less such as education, versus those that pay more (and where you find greater numbers of men), such as computer and engineering.
The author writes: “women sacrifice pay for all sorts of reasons including security, safety, flexibility, and fulfillment. Their priorities are vastly different than men’s. And when you account for that, when you compare apples to apples, when women actually make the same career choices as men, there is no gap. Men and women earn the same.” He adds that even when women pursue higher paying fields, such as medicine, they tend to gravitate towards areas that are less stressful, such dentistry rather than specialize in stressful positions such as surgery. Moreover, men work more hours.
While he acknowledges that women are having babies and do most of the child rearing — obvious factors that contribute to the gender pay gap — he claims that these are personal or societally-driven decisions and that truly, the glass ceiling has been broken.
Is this man living under a rock?!
I can rest on my laurels, throw a bunch of statistics in your direction and reinterpret the findings to provide evidence that the gender pay gap is a thing of the past. Or I can share the following proof that it’s not, that this author’s primary point, if you pay close attention to the article, has nothing to do with gender pay and more to do with his opinion that the Federal Government should not be wasting its time trying to equal the paying (pun intended) field.
That aside, let’s get down to brass tacks.
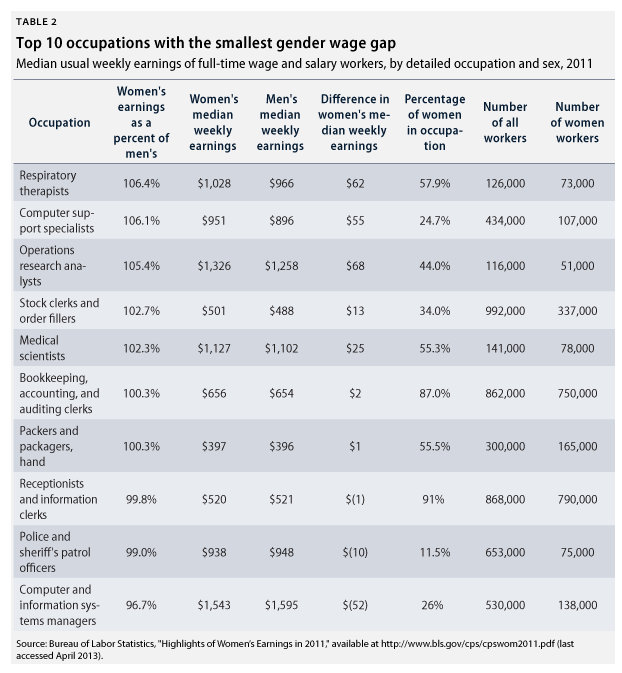
According to the latest figures from the Bureau of Labor Statistics, women continue to be paid less money than men in all but 7 of 534 occupations – respiratory therapy, computer support, operations research analysts, stock clerks, medical scientists, bookkeeping/accounting, and packager/package handlers. You can see the differences in the chart below as outlined by the Center for American Progress:
[Source: Center for American Progress]
Moreover, it’s not simply a matter of women choosing not to enter higher paying fields; often there is a discrimination bias taking place. For example, as Perry Hewett wrote in a 2011 Forbes.com piece, a key reason that women are lacking in tech is because this male-dominated industry is not broadening its professional networks to include more women. Anecdotally, I hear this all the time from my female techie friends. Importantly, the problem is magnified many fold among women of color who are trying the break the barriers. This problem is coupled with the need to improve girls’ access to science and technology programs (and boosting their interests in the same) so that we are producing a greater field of qualified applicants. And my gal pals also echo Hewett’s contention that visibility is a huge issue; even women who participate in more highly visible events are often invisible to the masses. Those who speak up are often ostracized when they do. The problem is pervasive.
In medicine, the reality is just as harsh. Although women are now entering medical school in droves, studies have suggested that gender discrimination is a large factor driving where females ultimately end up; in one survey, 75% of women on a surgical track had experienced gender discrimination. More specifically, female physicians have three choices in order to excel:
- deny that there is any distinction between her and her male colleagues, thereby joining the man’s clube and be subject to be treated as a “neuter”
- assume a more traditional societal role as a seductive, helpless, dependent female, which means she is then treated as a sex object
- become a superwoman and compulsive overachiever in career and family roles in order to supercede expectations in all areas of her life
As I’ve written previously, gender and age discrimination is also pervasive in the film and entertainment industry. I’m sure that there are more fields, more data, more anecdotes; I’ve simply scratched the surface with the most obvious. However, the issues underlying and driving the glass ceiling are complex. In some areas, women have shattered it; in the majority of others, it is intact. And to overcome the challenges we face as women, it’s more than simply leaning in, or making choices other than the ones that many women are forced to make.
The gender pay gap? It’s real and not going away anytime soon. And it will take more than empowerment to move the needle. I’m not entirely sure what the answer is. But when it comes to action, the future is now.
Read MoreWednesday Bubble: Two is the Magic Number?
When it comes to Traditional Chinese Medicine (TCM), is two the magic number? A variety of studies have examined the utility of TCM for menopausal symptoms and some have shown good benefit. However, does combining distinct forms of TCM yield better outcomes? Moreover, are these outcomes equal to those achieved by hormone therapy?
They may very well be, according to a small study that was presented this past May at the International Research Congress on Integrative Medicine and Health. Published in BMC Complementary and Alternative Medicine, the study explores the use of a Chinese herbal formulation named Kun Bao Wan alone and in combination with acupuncture and compares it to hormone therapy. Available in powder form and priced at approximately $8.00 a box, Kun Bao Yan is used in Chinese medicine to balance hormone levels, relieve insomnia and improve blood circulation to restore healthy metabolism. A web and database search yielded almost no information on side effects, reinforcing the need to work directly with a practitioner versed in Chinese medicine versus using it on your own.
Regardless, over a two-month period, 57 women in peri- or full on menopause took Kun Bao Wan (5 gm. twice a day) alone or in combination of 5 acupuncture sessions a month, or were assigned hormone therapy. During this time, symptoms (hot flashes, tingling, insomnia, nervousness, weakness, dizziness, palpitations) were measured with a scientifically validated index. The researchers also assessed hormone levels (FSH, estradiol) and symptom severity and frequency.
The findings appear to indicate that while all three strategies can significantly decrease menopause symptom scores, better results were achieved with Chinese medicine plus acupuncture compared to Chinese medicine alone, particularly in women who were postmenopausal. Additionally, Chinese medicine plus acupuncture was on par with hormone therapy with regards to its overall effects on FSH. Importantly, none of these strategies appeared to affect levels of circulating natural estradiol.
Granted, this study is quite small. But it does show that with Chinese Medicine, two combined modalities may be better than one. And are certainly on par with hormone therapy — and perhaps even safer.
Read More
Hot flashes, Traditional Chinese Medicine & JQF – it is time for an Rx change?
I am a huge fan of Traditional Chinese Medicine (TCM), having used various preparations over the past 20 years for numerous ailments. These preparations have been prescribed by a practitioner who is licensed and degreed in TCM and my experience, albeit anecdotal, has been nothing but positive. In fact, I have been using a TCM formulation for several years now to help battle numerous symptoms and in combination with other prescribed herbs, I’ve mostly won. That’s one of the main reasons that I am always intrigued when I stumble upon well-designed studies that demonstrate benefit, like this one in the journal Menopause.
A bit of context
TCM and other similar philosophies emphasizes various body systems that together, form a network or grid connected by a meridien, if you will, as well as the relationship of the body to its social and natural environment. Its primary focus on maintaining health and enhancing the body’s ability to fight off disease. TCM will not focus, for example, on treating specific pathogens but rather, on addressing non-specific factors that create disturbances or imbalances within a certain network. TCM also examines how these imbalances may occur in unique parts of a specific system, such as the heart and blood vessels and small intestine (all of which are part of the heart system) and how they change over time. Western medicine, on the other hand, focuses primarily on treating morbidities, or symptoms related to various conditions and diseases. You can read morerabout TCM in this post from last September.
In TCM, menopausal symptoms are believed to be related to a decline in yin or yang in the kidneys. One of the oldest prescriptions in TCM to reinforce kidney energy is known as ‘Qing E Fang’ (QEF) and the first record of its use dates back to the year 960. The preparation is a combination of four key ingredients that are mediated through estrogen receptors and expression, hence, its potential usefulness in menopause. (These ingredients, in case you are interested, are Cortex Eucommiae (whose bark and leaf have an antioxidant effect) Fructus Psoraleae (commonly used for bone health and to treat estrogen associated diseases), Semen Juglandis and Rhizoma Garlic.)
About the research
For this study, researchers used a formulation based on QEF known as Jiawei Qing’s Fang or, JQF, which used two of the four herbs (Cortex Eucommiae, Fructus Psoraleae) mentioned above. In JQF, they are combined with the herb, Salviae Miltiorrhizae, that has been used specifically to treat gynecological disorders and has properties that are similar to SERMs, drugs that mimic estrogen but are theoretically safer. The 72 women participating in the study were all perimenopausal and had severe and frequent hot flashes; they were randomly instructed to take JQF or placebo daily over 8 weeks. For a month thereafter, symptoms were evaluated using a menopause measure that looks at vasomotor, physical, psychosocial and sexual health). The women also kept daily diaries to record the frequency and severity of their flashes.
Notably, this is one of the first times that perimenopausal women have been the focus of a study that involves TCM. Moreover, in this study, researchers selected a formulation that worked on the kidney and also contained an herb that not only mimics SERMS but also improves blood circulation. And the findings? Women who randomly took JQF not only experienced significant improvements in their hot flashes, but also reported improvements in quality of life in terms of the impact of vasomotor and physical symptoms. Moreover, because Salviae Miltiorrhizae works on blood circulation, they also had reductions in the blood fats (triglyerides) which means that the formulation might also be beneficial in terms of heart disease prevention in menopausal women.
Is it time for a change of Rx for the change? Should you be seeking out a practitioner who can prescribe JQF and advise you on its best use for you? Or is it too early? JQF was well tolerated, although two women were found to have liver measures negatively affected in ways that did not require any medical intervention but did raise a few red flags and calls for more study. JQF represents a seemingly scientifically proven alternatives to hormone therapy. It’s refreshing to watch TCM come out of Asia and be increasingly incorporated into Western philosophy.
Hot flashes and Japanese herbal medicine: the lowdown on TU-025
Women who choose to go the alternative route for menopausal hot flashes have few evidenced-based options. Although acupuncture and standardized black cohosh have been shown to be effective in ameliorating hot flashes, others, including red clover and even soy, have been less successful. Consequently, herbal practitioners often turn to Traditional Chinese medicine (TCM) herbal formulations or the lesser known (in the U.S.) Japanese multiherb medicinal formulations known as Kampo. Interestingly, the term Kampo refers to ‘the way of China” and the practice which is several thousand years old is based on TCM.
Kampo is prescribed by over 90% of Japanese gynecologists and is regulated by the Japanese Ministry of Health to insure manufacturing standards and product stability. One of the most popular Kampo agents for perimenopausal hot flash management is an 1,800 year old formulaton known as “keishibukuryogan” or in the US, as TU-025. Comprised of a combination of cinnamon bark, peony root, peach kernal and mountain bark, it active ingredient remains unknown. Japanese data from both the government and the manufacturer demonstrate a very low incidence of side effects and no estrogenic activity, which means that theoretically, it could be safely used by women who have had breast or gynecologic cancers. Nevertheless, its utility in American women has not been known, at least until now.
In a study published in the August issue of Menopause, 178 postmenopausal women were randomly assigned placebo, 7.5 g/daily TU-025 or 12.5 g/daily TU-025 for 12 weeks. All participants reported 28 or more hot flashes a week, had been in menopause for at least a year, had stopped using hormones for at least 8 weeks if they were already using them, smoked less than 10 cigarettes a day and most were slightly overweight or obese (based on body mass index). None were using antidepressants (which studies have shown may help alleviate hot flashes), nor did they have a history of breast or uterine cancer. While the 7.5 gram daily is the dose taken most often by Japanese women, the researchers upped the dose to 12.5 gm daily to account for a larger sized American woman.
Read More