I’m so dizzy…
my head is spinning.
Those of you in my generation will remember this song by Vic Reeves with the Wonder Stuff. Talk about a one hit wonder! Or Vertigo, the incredible film by Alfred Hitchcock. But, dizziness is anything but wondrous and having suffered a form of vertigo that occurs when the head changes position (also known as benign paroxysmal positional vertigo or BPPV)), I can share that it’s an awful experience. The last time it happened, I didn’t leave the house, didn’t drive and required motion sickness pills to sleep.
The reason why I’m sharing this with you is that BPPV occurs in at least twice as many women as men and its likelihood increases with aging. More troubling is the fact that study findings suggest that hormonal fluctuations — especially during menopause — appear to play a role. Historically, BPPV has been linked to the dislodging of crystals in the inner ear, which causes a greater sensitivity to gravity. Thereafter, changes in head position, for example, lying down, looking up or turning over in bed can cause brief vertigo spells. Although most of the time researchers don’t know why it occurs in some people versus others, BPPV has been linked to head trauma other ear conditions.
The most current research comes from a study of over 1,300 individuals, almost 1,000 of whom were women. I’ve already noted that in the general population, BPPV occurs in twice as many women as men. In this population, not only were women in the 40s three times as likely as their male peers to develop BPPV, but most of them reported being in perimenopause, suggesting that hormonal fluctuations , especially estrogen, were at play. What’s more, some data suggest that there is as we age, there is a deterioration in the protein that help anchor the inner ear crystals, and estrogen appears to help promote this.
The silver lining is that while there is little that can be done about aging and estrogen’s role in BPPV, the problem can be successfully addressed with a series of head maneuvers that help restore the crystals back to their former position. Still, I personally find that I get periodic vertigo sensations at the oddest times and that they tend to worsen during my worst hormone movements.
Dizzy Lizzie? Sure, I’ll admit to it. What about you?
Read MoreGot Low T? Low E? What?!!!
Do you recall the Low T campaign, you know, the one where Daryl Moose Johnston is able to ‘get back in the game’ once he starts correcting his testosterone deficiency? Well, not only is Darryl suffering from low testosterone levels but newly published research suggests that men like Darryl may also be suffering from ‘Low E,’ as in estrogen. Can you hear the ‘cha ching’ in the background yet?
As researchers continue to unravel the mysteries of how declining testosterone affects men, they’ve discovered that testosterone has a partner in crime: estrogen. In fact, not only does it appear that different men need different levels of testosterone in their body to maintain their lean/fat mass balance, muscle strength and size, but as testosterone levels begin to decline as men age, so does estrogen and with it, men may be left with the accumulating middle tire that many of us women are quite accustomed to. Moreover, findings from the study mentioned above show that both testosterone and estrogen regulate sexual function in men.
A bit of context here just so we are on the same page. This recent bit of information comes from a study of 198 men between the age of 20 and 50 who were healthy and had normal testosterone levels. In men, ‘normal’ equates to ranges that decline as they age. The estrogen component is a bit trickier to explain; more than 80% of circulating natural estrogen in a man’s body comes from the conversion of testosterone. So, as testosterone levels start to decrease, so do estrogen levels. And, when some of the men in the study were provided with a steroid agent that blocks that conversion, they experienced an increase in body fat percentage. Another important point was that fat began to accumulate at testosterone levels well above the levels that would affect muscle strength and size, i.e. 300 to 350 ng. Finally, in both groups of men — those who received various levels of testosterone and those who received various levels of testosterone and a hormone to prevent conversion to estrogen — declines in desire and erectile function similarly declined as testosterone did.
Back in March, I wrote a post about hormone deficiency in men and following the money trail. Mind you, declining levels of testosterone (and by default, estrogen) can have significant consequences for some men that go well beyond sexual dysfunction or a bit of body fat. Consequently, by conducting this research, scientists will be better able to help men whose testosterone levels fall below a certain point, although estrogen replacement comes with its own set of problems (enlarged breasts anyone?). Aside from the obvious benefits, such as a better strategy for interpreting testosterone levels, identifying any negative consequences that might be associated with them and treating them accordingly, one has to wonder if the conversion of testosterone to estradiol or lack thereof, is a harbinger for a future campaign.
Got low T? Got Low E?
Need I say more?
Read More
Newsflash: So, estrogen is safe?
 If you’ve been following this blog for any period of time, you know that I’ve consistently shared data that demonstrate the hormones, particularly combination hormone replacement therapy (HRT) can be dangerous, depending on age, time since menopause and other concomitant health issues. Yet, the medical community continues to beat the dead horse of trying to prove the hormone replacement in any form has a role in women’s health. And because I have promised to share the facts, regardless of whether or not I have questions about the motivation underlying their derivation, I am writing this post.
If you’ve been following this blog for any period of time, you know that I’ve consistently shared data that demonstrate the hormones, particularly combination hormone replacement therapy (HRT) can be dangerous, depending on age, time since menopause and other concomitant health issues. Yet, the medical community continues to beat the dead horse of trying to prove the hormone replacement in any form has a role in women’s health. And because I have promised to share the facts, regardless of whether or not I have questions about the motivation underlying their derivation, I am writing this post.
According to research appearing in the July 28 online issue of the American Journal of Public Health, estrogen actually prevents deaths among women who have had hysterectomies. By the way, that’s estrogen ALONE, not estrogen plus progestin, and that is a critical distinction.
Onto the findings. When researchers took another gander at the Women’s Health Initiative data, they sought to determine how the rate of excess mortality among women who took placebo versus those who took estrogen over the course of the landmark study actually translated into premature deaths that might have been preventable. And what they found is pretty shocking:
- The researchers looked at deaths in women who had undergone hysterectomy and still had an ovary intact compared with those who did not have any ovaries (note that sightly more than half — 54% — of women have both ovaries removed at the time of hysterectomy)
- They also examined the use of oral estrogen among the 50 to 59 year old set between the years 2001 and 2004, noting a decline by as much as 60% (largely the result of the the findings of the Women’s Health Initiative) and a relative decline by as much as 71% by the year 2009.
- In composite, they were able to calculate that between 2002 and 2011, a least 18,601 excess deaths occurred and as many as 91,61o excess deaths occurred among women who had had hysterectomies and chose not to use estrogen. This translates to an actual toll attributed to the decision of 40,292 to 48,835 deaths.
The researchers say that estrogen therapy alone reduces mortality mainly by reducing the number of heart disease-related deaths; notably early surgical menopause and complete removal of the ovaries boost the risk for coronary heart disease. Estrogen prevents the development of atherosclerosis and helps maintain normal blood flow.
It’s important to remember that these findings do not apply to women younger than age 50 or older than age 59. Moreover, they also fail to consider other reasons for the increase in heart disease among women as their estrogen declines, such as a surge in cholesterol. And, despite the improved odds against dying from heart disease, these data also ignore other health issues associated with estrogen alone, such as incontinence, hip fracture and of course, breast cancer among certain subsets of women. Hence, again, I am forced to ask the question why researchers continue to beat this horse to death when the deaths prevented may carry the cost of other issues?
I don’t believe that this is anything that will be resolved any time soon. And, as I have written previously we’re drowning in politics, medicine and industry. And it’s difficult to discern truth from fiction, data from data, risk from benefit. Ongoing analyses will eventually reveal what’s what. Meanwhile, read the library of HRT posts on Flashfree. Talk to your physician. Avoid hasty decisions. And consider alternatives. If the medical community can’t agree, perhaps it’s time to put down the gauntlet and wait out the firestorm.
The choice is yours’. Which side are you willing to err on?
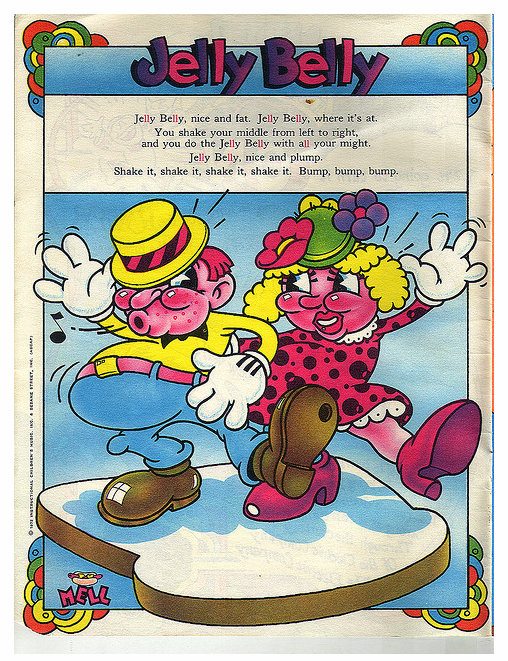
Read MoreJelly in yo belly?
[The Electric Company – Retro-style illustrated lyric page for “Jelly Belly.” Art by Mell. From the Electric Company Original Cast album booklet, 1972. Courtesy: 4-Color Cowboy Vintage Print Collection]
Sigh. I’ve written about this, I’m experiencing it, heck, I’m stumped.
Belly fat.
It’s a well-known fact that many women’s fat storage begins to shift as they go through menopause. However, many women are unaware that this fat storage pattern is downright dangerous, dramatically increasing the risk for conditions like diabetes, heart disease, stroke and even some cancers.
While experts have made the connection between declining estrogen levels and an increase in fat deposits in the mid section, they have not entirely understood how it happens. That is, until now. Indeed, when researchers from Concordia University in Canada and the Mayo Clinic joined forces, they discovered that cells are the culprit. Yup, cells.
Let me explain.
Professor Sylvia Santosa, the leading investigator, says that she and her colleagues undertook the investigation because of the dangers associated with belly fat in postmenopausal women, noting that she felt that it was important to understand how low estrogen levels redirect fat storage. Consequently, she compared fat storage in 12 premenopausal and 11 postmenopausal women who were, on average, roughly 50 years old. To insure accuracy, the women all consumed the same meals for 5 days before the study and were matched by age, weight, and similar body weight, BMI and body fat compositions. They also examined the activities of fatty acids and certain enzymes that promote and alter fatty acids so that they wind up stored in the last place we’d like them to be stored: our bellies.
What they discovered is that twice as many dietary fatty acids — the type found in meals instead of the type that flow freely in the bloodstream — were being deposited into abdominal storage in postmenopausal that premenopausal women. The reason for this doubling was that the decline in estrogen appears to increase a certain protein in tissue that stores fat in the belly, and that its partner in crime – an enzyme had as much as 40% higher activity in postmenopause.
To put it in plain English: the overall fat storage machinery in postmenopausal women is faulty. Not only are we storing more fat than ever before, but our cells also don’t want to let go of it. Yikes!
While researchers continue to tease out the culprits so that they can figure out how to optimally target them, we are left with a dilemma: what now? Short of changing your diet and re-upping your exercise, or paying for fat extraction, there’s not a whole lot of ‘what.’ Unfortunately, many of us may need to live with the jelly belly the best we can.
Read MoreWednesday Bubble: U.S. Preventive Services Task Force Recommends Against Use of Hormone Therapy for Chronic Disease Prevention
I just can’t help myself. It’s Monday. But this news item calls for a Wednesday Bubble. And yet another nail in the HRT coffin.
The U.S. Preventive Services Task Force (USPSTF) issued an update to its 2005 statement on hormonal therapy late this afternoon. It reads:
“The U.S. Preventive Services Task Force (USPSTF) recommends against the use of of combined estrogen and progestin for the prevention of chronic conditions in postmenopausal women” (evidence grade D – There is moderate or high certainty that the service has no net benefit or that the harms outweigh the benefits).
“The USPTF recommends against the use of of estrogen for the prevention of chronic conditions in postmenopausal women who have had a hysterectomy (D recommendation).
Wondering what this means?
The USPTF recommendations are clear that they refer to the use of HRT and hormone therapy for the purpose of reducing a woman’s risk of developing certain chronic diseases, such as heart disease or dementia and not for the purpose of treating considering hormone therapy for menopausal symptoms such as hot flashes or vaginal dryness/atrophy. However, they are also clear about the data that explores the use of hormone therapy for chronic diseases, noting that while combined HRT has been shown to decrease the risk for fractures, this decline is accompanied by an increase in the risk for serious events that include:
- stroke
- invasive breast cancer
- dementia
- gallbladder disease
- blood clots in the veins or lungs
Additionally, they report that data do not demonstrate a decrease in heart disease and even show an increased likelihood — 1.22 times the norm — for some type of heart event.
For estrogen alone, they again note the benefits in terms of fracture reductions and even a small decline in risk of developing or dying from invasive breast cancer (e.g. 8 fewer cases or 2 fewer deaths per 10,000 person years). However, estrogen-alone has also been associated with “important harms” including:
- stroke
- blood clots in the veins
- gallbladder disease
Like combined hormone therapy, estrogen alone does not reduce the risk for coronary heart disease.
The Task Force also points out that both forms of hormone therapy have been associated with an increased incidence of stress, mixed or urge urinary incontinence after one year.
Mind you, naysayers will say that the average age of women participating in the Women’s Health Initiative were a bit older than the vast majority of women who are transitioning through menopause. To a certain extent, the Task Force agrees, calling for “new research to help better define whether there is a differential balance of benefits and harms based on age at initiation, duration of use and dose or delivery mechanism. Still, they conclude with “high certainty that there is zero to negative net benefit for the use of combined estrogen and progestin therapy for the prevention of chronic conditions and concludes with moderate certainty that there is no net benefit for use of estrogen alone.” Moreover, major health organizations are aligned with the new recommendations. For example, the American Heart Association and American Congress of Obstetricians and Gynecologists recommend against using hormonal therapy to prevent heart disease. The Canadian Task Force on Preventive Health Care and American Academy of Family Physicians are totally aligned with the USPSTF in terms of the use of hormonal therapy to prevent chronic illness in postmenopausal women. Even the North American Menopause Society, a huge proponent of hormone therapy, does not believe that hormones should be used to protect the heart or prevent dementia.
Let’s place the recommendations in context.
By the time most women reach menopause, they are expected to live at least 30 additional years. During this time, they have varied risks for developing chronic diseases, ranging from 30% for coronary heart disease and 21% for stroke to 22% for dementia and 11% for breast cancer. In an accompanying press release, Associate Professor of Medicine and of Epidemiology and Biostatistics at the University of California, San Francisco , Dr. Kirstin Bibbins-Domingo, says “the Task Force recommends a number of important preventive measures women can take to prevent chronic diseases, including quitting smoking and identifying and treating high blood pressure and high cholesterol. There are also other effective ways that women can reduce their risk of bone fractures, such as weight-bearing exercise and being screened and treated, as appropriate for osteoporosis.”
In other words, speak to your practitioner about evidence-based strategies to maintain good health and prevent disease. In this case, the evidence for HRT in disease prevention efforts during menopause is scant and the risks appear to outweigh the benefits.
Read More