Wednesday Bubble: My Fitbit Flex
I have been meaning to share my experiences with the fitbit flex every since it arrived in my mail two months ago. Fortunately, a FaceBook thread debating the merits of wearable mobile health devices prompted me to finally sit down and gather my thoughts. True confession: this my personal opinion and nothing more.
The fitbit flex. Pretty nifty, right? However, anyone who knows me well will want to know why I purchased one in the first place; after all, I hardly need motivation to go to the gym or get on my bike.
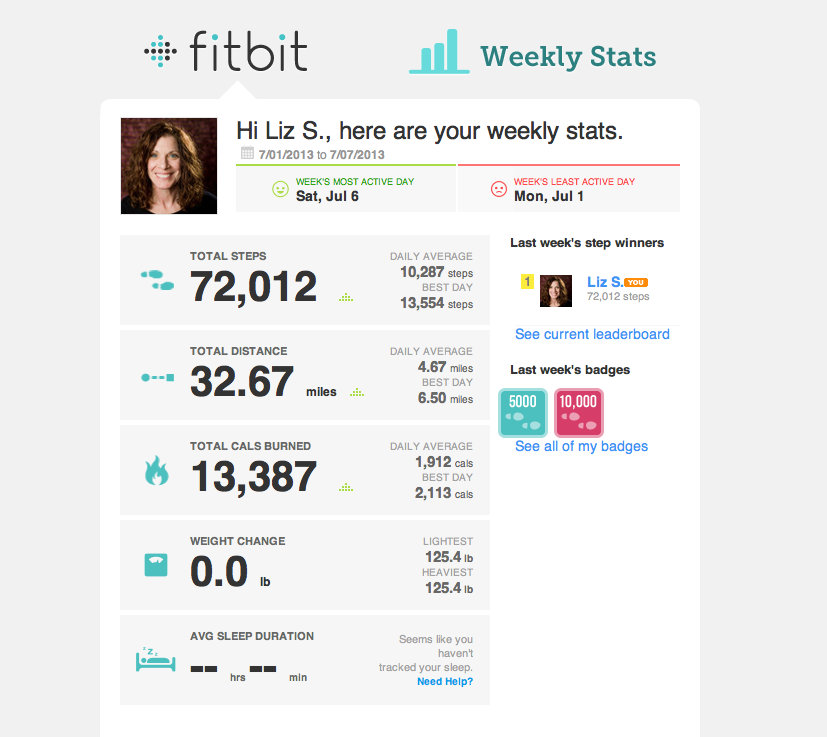
Weight gain. That’s right, weight gain (disregard the number below – it’s not reflective of what I am referring to). And while a few pounds is hardly cause for concern, those of you in the midlife set will understand that some of the changes that take place in our bodies don’t always bode so well. Hence, I decided to take charge, contacted an RD to discuss my eating patterns and decided to monitor my activity a little more closely. The rub? The flex doesn’t really monitor one’s activity very well.
In fact, if you are not upright, it may not monitor your activity at all. That takes a bit more motivation to take the time to input your activity, time spent doing the activity, etc, time that might be better spent actually doing more of that activity.
If you look at my numbers over the past week, they look pretty good:
However, this is what they don’t show:
- Hours spent on the recumbent bike: 5
- Hours rowing: 2
- Hours gardening: 2
- Hours spent doing housework: 3
They also don’t account for the fact that the battery ran out of juice a few times and I had to take the flex off for a recharge.
Moreover, after the first week, I stopped monitoring my sleep. It didn’t appear to be very accurate. And calories consumed or burned? Fuhgeddaboutit! If the band is not accurately reflecting my activity and I am not inputting any information about the food I’m eating, it’s hard to accurately determine how many calories I am burning, right?
Is there anything that I like about the flex?
It’s lightweight and I usually forget that I’m wearing it. That’s a lovely feature. I think it’s cool and although the weekly reports are not quite right, it’s still nice to know that I have daily goal — 10,000 steps — that I am trying to reach if not surpass. However, as a tool to effectively monitor what I am doing and how I’m doing? The flex gets about a 3 out of 10 in my book. I want easy, accurate and intuitive. I want a device that thinks for me and not the other way around. Clearly, when you only spend $99 you are getting a Nissan and not an Infiniti. But, if you are going to drop the dollars in the first place, shouldn’t you know what you are buying?
Admittedly, I ordered the flex before it became available. As an early adopter, I guess that I got what I paid for: no guarantee.
On the flip side. I know that anecdotally, those of my friends who have difficulty motivating themselves to move more have been inspired by the flex and other mobile health devices. Moreover, data from one study demonstrated that users of a smartphone monitoring application were likelier to both log steps regularly and had a greater odds of exceeding the designated 10,000 step goal per entry. Less clear, however, was whether or not these changes in behavior would take hold permanently or were simply an anomaly of the shiny new object syndrome.
Already, I find myself losing interest in the flex and will likely abandon it over time. I find that I am no longer motivated to log in the extras that the flex can’t record. An hour with my personal trainer would have likely been a better use of my money.
What about you? Do you have a flex or some other device? What do you like about it or dislike about it? Are you more or less motivated now that you have a device or will it end up in the land of lost tech toys?
Inquiring minds…
[Disclosure – Fitbit did not approach me with a suggestion to purchase a flex or write a review. The words, thoughts and opinions expressed are solely mine without bias or intevention.]
Read MoreSleep and mindfulness
Up to 63% of women are affected with sleep issues, in particular insomnia, during and after menopause. It’s no wonder that I can’t stop writing about sleep. And, while there are numerous hypotheses as to why insomnia, i.e. difficulty falling asleep or staying asleep more than three times a week (or, not having refreshing sleep just as frequently) affects women during the ‘pause more than at other times in their lives, relief appears to be more than a few zzz’s away.
Can mindfulness-based interventions help?
Research suggests that by focusing on our mental and physical state of mind when experiencing insomnia, we can then learn how to shift mental processes to achieve a better balance. This is exactly what meditation does; increasing attentiveness and focus has been shown to alleviate stress and promote wellbeing.
When researchers compared the degree of attentiveness, alertness, determination and concentration between women with and without insomnia, they found that that women with insomnia appeared to report having less mindfulness, were less attentive when performing tasks or eating. Moreover, the degree of mindfulness or lack thereof did not appear to be affected by mood or by menopausal symptoms, factors that could also affect sleep.
Ultimately, the path towards better sleep may be paved with the ability to improve mindfulness, to actively engage and gain control over cognitive resources that we aren’t even aware we are using. At its most basic level, it simply means that meditation may help make to improve awareness over our perceptions so that we can increase our ability to respond to events with a broad range of options, instead of giving in to the storm of thoughts and emotions.
Increasingly, I am finding myself drawn towards a meditation practice. Do you meditate? What types of benefits have you noticed?
Read MoreSisters, friends…keeping the communication channels open
When life piles, who do you turn to? Your sister? Your friends? The internet?
Without them I would be lost.
When I first started penning this blog, I ran across a small study. While many in scientific circles would refer to it as a pilot study, with findings that are inconsequential because of the small numbers, I am here to declare loudly and broadly that small and anecdotal sometime rule the day!
What type of resources do you rely on? And where do you turn for information or support? And, who should you turn to when available information is seemingly overwhelming and inconsistent, and medical expertise is unavailable?A friend recently commented that the type of resources available to women living in rural areas are very different than those available to women living in urban areas. Hence, the ability to access knowledgeable practitioners or even find trusted sources of information really depends on where you live.
This has been borne out by results of a study conducted among 25 menopausal women living in rural areas of Nova Scotia. Participants described a need to understand the intensity of their symptoms but often found it difficult to sift through “excessive and conflicting” information on the web. This was further compounded by the lack of trusting relationships with healthcare providers due to their scarcity and also, the fact that local facilities failed to retain good people.
The researchers explain that women who participated in this study drew heavily on shared experiences and the ability to communicate freely and openly with women who were going through similar things. More often than not, they continuously sought validation from their peers to avoid feeling confused and alone. And found that a great way to deal menopause was through humour.
Whether a woman resides in rural Nova Scotia or New York City, a sense of community, mixed with open communication and a little bit of humour, can go a long way. She who laughs with others…lasts.
Read MoreNewsFlash: ‘First’ Non-Hormonal Treatment for Hot Flashes – Brisdelle
It’s very important when you see news headlines that you read between the lines.
This came across my mailbox earlier in the week:
Noven Receives FDA Approval for Brisdelle™ (Paroxetine) Capsules, the First Nonhormonal Therapy for Vasomotor Symptoms Associated with Menopause
So, let me explain.
Brisdelle is the first non-hormonal treatment for menopause to receive FDA approval. But, it’s not the first nor the only nonhormonal treatment for vasomotor symptoms; heck, one glance at the tag cloud or the archives and you will see that there are lots.
Claim aside, it’s important to break down the news for you.
Brisdelle is a low-dose form of Paxil, an SSRI antidepressant. Because of its dosage, it is only indicated for treatment of hot flashes and night sweats, and not for depression, obsessive compulsive disorder and anxiety.
This is what I wrote late last year when Noven first presented study findings to the North American Menopause Society:
Paroxetine is not the first antidepressant to be studied in menopausal women and you may recall that I wrote about the use of Lexapro for hot flashes about two years ago. You can find that post here. However, paroxetine is the antidepressant that’s all the buzz right now, since Noven Pharmaceuticals presented two studies last week at the North American Menopause Society annual meeting. Note that it’s been reframed as ‘low-dose non-hormonal therapy for menopausal vasomotor symptoms,’ but ya still gotta call a spade a spade and what it is is an antidepressant.
In one of two studies, 568 women (40+ years of age) who experienced 7 to 8 moderate or severe hot flashes on a daily basis of 50 to 60 on a weekly basis took either 7.5 mg of LDMP or placebo daily over six months. By the end of the first month (and in contrast to the study’s start), women who were taking LDMP experienced 28.9 fewer hot flashes per week (compared to 19 fewer per week for women taking placebo pills). By the third month, this increased by roughly 10 fewer per week in both groups. The severity of the hot flashes also significantly decreased. Safety wise, women taking LDMP reported nausea and bronchitis.
In the complementary study, which lasted for three months, 606 women in the same demographic took the same dose of LDMP or placebo. Decreases in mean number of flashes per week were pretty much on par with the first study (33 compared to 23.5 for placebo) and similarly, a trend towards maintaining and growing benefits were observed. Severity of hot flashes also declined but by the study’s end, were not significantly different than placebo. This time, women who took LDMP most frequently reported dizziness and fatigue.
Dr. James Simon, one of the studies’ investigators and a professor of ob/gyn at GWU School of Medicine claims that symptoms of menopause often go untreated when women are unable or unwilling to take hormone therapy, which is not entirely true. Another investigator — Dr. Andrew Kaunitz from the University of Florida College of Medicine in Jacksonville notes that if LDMP is approved by the FDA, “it could be the first nonhormonal option available for women.” Again, this statement is not entirely true. LDMP has the potential to become the first nonhormonal treatment APPROVED by FDA for vasomotor symptoms in menopausal women. There are other options out there but on the most part, they are not embraced by Western practitioners. Take note: while many Western practitioners will argue until they are blue in the face that alternative strategies have no role, are no better than placebo, and do not have evidenced-based trial data to support their use, they are simply incorrect. An unequivocal statement about every alternative strategy available to wo-man is bad medicine at best and at worst? Sheer ignorance.
Back to LDMP…LDMP appears to effectively diminish hot flashes and sweats but it is not without side effects. And while the dosage is considerably lower than full-strength antidepressants, we don’t have enough information to know if it will ultimately mimic its higher dose partner; the most common side effects reported in these trials are the very same that have been reported with Paxil. Another common side effect of Paxil is the effects on libido and it is a well known fact that as many women go through menopause, they experience declines in sex drive, lubrication and the ability to reach orgasm. In the pivotal studies used to gain approval, about half of the women appeared to have sexual dysfunction; what’s unclear is whether or not the cause was the drug or menopause itself. Another important point that is missing from this story is that back in March, the FDA’s advisory committee on reproductive drugs voted against approval, stating that paroxetine’s effectiveness in reducing hot flashes was underwhelming and not unlike that seen among women taking placebo in clinical studies.
I applaud Noven for its efforts to offer an alternative to HRT, one that has been approved by the FDA. However, the way that communications about this agent are being framed, it appears that the spin masters are working overtime. It’s essential to understand that this treatment is non-hormonal but still a pharmaceutical agent. And while I am a huge proponent of antidepressants for depression, I remain skeptical that they are the best agents for addressing menopausal symptoms. Cost may be an issue – no word on the price point as of yet.
I guess that time will tell.
Read More
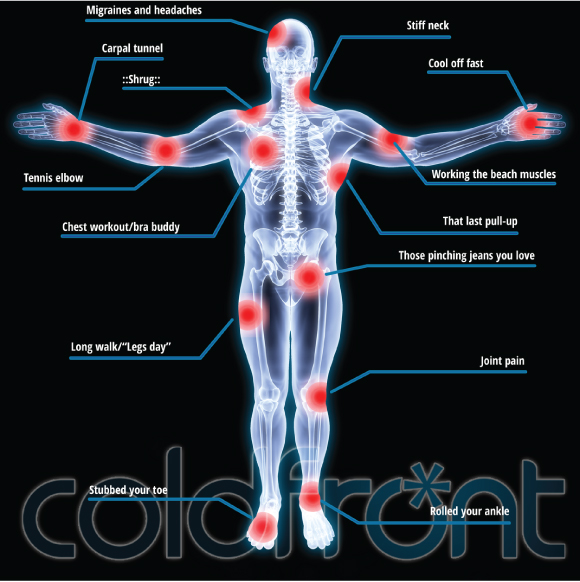
Redefining ‘cool’: Cold Front’s pushing new boundaries
Cold Front ® is not simply for hot flashes any longer. In fact, entrepreneur and Founder of Personally Cool — Susie Hadas — is expanding her horizons and needs your help!
Although hot flashes may be the only game in FlashFree Town, there appears to be a need for cooling outside the menopausal boundaries. And let’s face it; as much as me and several other esteemed menopause bloggers have tried to move the needle, talking menopause is not always easy. And engaging women who want to admit that they’re not simply sweating but flashing can be an upward battle. Consequently, Susie and her team have gone back to the drawing board and emerged with a brand new bag: personally cooling is truly a global endeavour. Voila! A new Indiegogo Campaign has been born! And your assistance is needed!
I can assure you that Susie is not turning her back on menopause but looking forward to help millions of individuals worldwide who suffer from:
- heat intolerance due to multiple sclerosis and thyroid issues
- hormonal changes in men that also cause hot flashes
- chemotherapy side effects
When I caught Susie on the Twitter stream announcing the campaign, I sent her a note asking for more details. She says that when she and her team were on the road, “more people were talking to us – travelers, moms, fashionistas, runners, bikers, hikers, the list goes on. They were all asking us the same question, “Why aren’t you talking to me?” So, she took a step back and decided to relaunch Cold Front on a new level.
Susie notes that in order to grow, they need funding. Moreover, the money they raise to produce another run will enable the company to produce wraps for the gel packs and a single larger gel pack which is what customers have asked for.
And yet, there is another element to this that I want to share with you:
Giving back.
Like many entrepreneurs, Susie has not rested on her laurels or profits and rather, has consistently and continually given back. An attractive aspect of the Indiegogo campaign is that the money that you donate can actually go towards funding three charities whose constituents will benefit from cold therapy:
- Love to Langa, a Cape Townships, South Africa organization that is working to build and renovate Early Childhood Education Centers. Your gift of coldfront® will cool the children down and always be on hand as a non-toxic first-aid solution for minor bumps and bruises.
- Nayaya Health, a Nepal-based organization that provides care to residents of the Achham region of Nepal for free, and employs over 160 Nepalese citizens. (Nyaya Health has been using coldfront® to keep staff and patients cool and aid in pain relief and they have requested more units).
- CT Challenge’s Center for Survivorship, a Connecticut-based survivorship center offering evidence-based programs designed to help empower cancer survivors to live healthier lives.
Susie’s campaign goal is $100,000 and she’s got 35 days left to achieve it.
How about we chip in as a team and cool the world?
Read MoreWednesday Bubble: Want to lose weight? Set better goals!
I can only imagine that you are rolling your eyes at the headline. But according to newly published research, how you set your weight loss goals may ultimately determine how successful or not you are at realizing them.
Let me break it down for you:
Menopause is challenging enough when it comes to weight gain and belly fat and the rest. However, are we setting ourselves up for failure when we tell ourselves that we want to lose “3 lbs?” Researchers from Florida State University and Washington University say a resounding “yes!”
They say that there is a distinction between making high-low range goals (I want to lose 2 to 4 pounds) and single number goals (I want to lose three pounds this week). This distinction makes an enormous difference, at least in terms of reengaging, i.e. doing something once and then doing it again — either by setting the same goal or setting. The high-low option actually offers an out, so to speak or as the researchers state “best of both worlds.” In other words, it’s a win-win whether or not you lose one pound or three pounds; both fall into the range that you set at the start. Conversely, a single number sets us up for ‘all or nothing’ or as I like to say, all or nothing in between. After all, isn’t is amazing when you set up to lose a pound and end up with a two pound bonus?!
To test out their hypothesis, the researchers 45 adult women around 45 years of age to establish a single number weight loss goal or high-low weight loss goal for a week over three weeks. During this time period, they attended one hour group sessions and learned about healthy lifestyle practices and weight loss was measured weekly. After three weeks, they had the option of reengaging for another 10 weeks. To avoid generalization of findings, the study was also repeated but this time, the goal had to do with overeating a regular sized bag of M&Ms and focused on achieving a target number.
So, how did the participants do?
In the weight loss study, more patients setting high-low goals reenrolled in the second portion than those setting single number goals. In the second study, the high-low goal left the participants with greater levels of accomplishment and a significantly greater interest in reengaging in goal setting again.
The key? Attainable and challenging.
Look, these numbers are small and not definitive. But it should make you stop and pause: is the way that you are setting your weight goals setting you up for success or failure? Interesting question, right?
Read More