Breast Cancer & Physical Activity: What’s the 4-11?
 Want to reduce your breast cancer risk? According to new study findings published in Cancer, Epidemiology, Biomarkers & Prevention, at least an hour of moderate to vigorous daily activity may significantly reduce breast cancer risk in postmenopausal women. That’s just an hour a day or at least seven hours a week.
Want to reduce your breast cancer risk? According to new study findings published in Cancer, Epidemiology, Biomarkers & Prevention, at least an hour of moderate to vigorous daily activity may significantly reduce breast cancer risk in postmenopausal women. That’s just an hour a day or at least seven hours a week.
However, is it really that simple? Moreover, are there other factors at play that influence risk such as hormone receptor status, body mass index, weight gain or use of postmenopausal hormones? Notably, all of these have been linked with an increased cancer risk.
Indeed, when the researchers evaluated information provided by over 73,000 women (ages 50-74) over a course of 12 years, they were able to confirm what has eluded medical science for years: even moderate intensity activity, i.e. walking, when conducted daily, can have a major impact on breast cancer risk. Participants were asked to report, via questionnaire, the average number of hours they spent walking, jogging, running, lap swimming, tennis/raquetball, bicycling, doing aerobics or calisthenics and dancing. Assessments were also made on the number of MET hours — metabolic equivalent hours — were expended. Finally, adjustments were made to the findings that accounted for possible confounding factors, things like education, adult weight change and BMI, smoking and alcohol, age at menopause, personal history of breast cysts, hysterectomy or oopherorectomy, family history of breast cancer and finally, use of any type of hormone therapy and if use was current.
On average, women expended 9.5 MET-hours/week, which is equivalent to 3.5 hours/week of moderately paced walking. Additionally, 47% reported that walking was the only recreational physical activity that they participated in. Overall, these women tended to be leaner, more likely to lose or maintain their weight, more likely to drink alcohol and less likely to be current smokers. Importantly, they were less likely to use hormone replacement. And, compared to more vigorous physical activity (>42 MET-hours/week), women who reported walking at least an hour day were found to have a 14% lower risk for breast cancer; their more active peers almost double this – or a 25% lower risk. These findings remained even after the researchers made adjustments for the factors mentioned above – body type, hormonal status and estrogen receptor status.
In a related press release, a senior epidemiologist with the American Association for Cancer Research and a study co-author, Dr. Alpa Patel, points out that “current guidelines recommend that adults should strive to get at least 2.5 hours per week of moderate intensity activity or 75 minutes per week of vigorous intensity activity for overall health.” Yet, less than half of U.S. American women are active at these levels and the researchers note that an even smaller proportion are likely to achieve the higher levels necessary for breast cancer reduction. And yet, just an hour a day of moderate intensity walking can have a positive impact.
I cannot stress this enough: get off of your butts and walk. It doesn’t take a gym membership or a major equipment investment. And, it may actually prevent breast cancer!
Read More
Early menopause – is there a silver lining?
Early menopause (menopause before age 40) is often viewed as a kiss of death, especially among women who desire children (or more children) or rightly feel that it’s not yet ‘their time.’ More importantly, early menopause has been linked to a number of serious health conditions, including osteoporosis, heart disease and osteoporosis. But there is good news in the mix: it appears that early menopause may possibly reduce the risk of breast cancer in women under the age of 50. In fact, in a study aptly named the Two Sister Study, researchers compared 1,422 women with breast cancer who were diagnosed before age 50 and 1,669 case ‘sisters’who were free of breast cancer. The women were asked if they had experienced hot flashes, poor sleep, night sweats, irritability or depression and were asked specifically about the age when these symptoms first began. All participants were similar with regard to race, education, childbirth, breastfeeding experiences, cigarette smoking and alcohol intake.
Almost a third of the women who had menopausal symptoms before their they were either diagnosed with breast cancer or before their first interview. These women were likelier to have had a hysterectomy. And 30% who had hot flashes before the average age also reported that they had used hormone replacement therapy. Most importantly, however, women who had menopausal type symptoms before the age of 50 had half the odds of their peers of developing breast cancer, in particular, estrogen-positive breast cancer. This protection tended to decline the older that women became.
What do these findings mean? Undoubtedly it is important to consider factors that could influence the findings, such as age at first menopause or first birth, BMI, use of hormones, drinking and smoking. None of these variables appeared to affect the results. Second, self-reports are sometimes not entirely accurate yet the researchers accounted for this bias in their analysis.
So, today, I am reporting some quite good news. Early menopause can be devastating. But it may confer important protection against breast cancer and that is a very good thing!
Read MoreWednesday Bubble: Hold Your Breasts; it’s Breast Cancer Awareness Month
Got pink? In case you haven’t noticed, it’s Breast Cancer Awareness month.
Want to take good care of those bewbs of yours’? Check out this incredible post by blogger and cancer advocate Jody Schoger. I’ve known Jody virtually for a few years now and I am consistently impressed by her efforts to educate and not simply raise awareness.
Take note! As Jody writes:
“The first week of Breast Cancer Awareness has ended. Sometimes it reminds me of how Christmas has been commercialized – it starts early, is in your face, and makes myth of the experience itself. It can trivialize a serious disease, divert discussion and dollars. I happen to think if we continue to act fearlessly – as friends, as survivors, advocates and activists – in bringing our intellecrtual collective to bear on the issue we can change the landscape for your daughters. Last week I was stunned to hear someone on our weekly #BCSM chat express the thought that we – co moderators Alicia Staley and Deanna Attai, MD and I — had a political agenda. If having an anti-cancer, evidence-based, pro-survivorship, community-based agenda is political then yes, I’ll be the first to print campaign buttons and banners. On my dollar. Not from pimping cancer.”
Jody has a lot more to say so please, visit her blog before you do anything else today. And take care of your health by informing yourself in a thoughtful way. “Anti-cancer, evidence-based, pro-survivorship?” Right on, Jody!
Read MoreNewsflash: Estrogen only joins “avoid long-term hormone therapy use” recommendations
How many times does one need to get hit over the head before they have that “ah-ha” moment?
That’s pretty much the party line when it comes to hormone replacement therapy, or HRT. I’ve been writing about HRT since I started this blog. And I have been reading study after study that ultimately come to the same conclusion: long-term use of any hormones is unsafe.
I know that there are naysayers out there who don’t want to believe. Even the International Menopause Society continues to dispute the link between combined hormones and breast cancer. Yet, I wholeheartedly believe in free will and choice, informed decision-making needs to lead the way when it comes to your health.
And so, in the latest wrench to be thrown into the HRT argument, researchers from Brigham and Women’s Hospital in Boston, reporting from the annual American Association for Cancer Research meeting, that the longer that any hormone replacement is used, regardless of whether or not it is estrogen plus progesterone or estrogen alone, the higher the risk for developing breast cancer.
Did you read that?
Lead researcher Wendy Y Chen is quoted in the Association’s newsrelease as saying that while it’s “already been confirmed that patients shouldn’t be undergoing estrogen plus progesteron hormone therapy for the long term,” (you can read about that here), “what we found is that people should also be careful about longer-term use of estrogen-alone [hormone therapy].”
Chen and her team evaluated data collected during the Nurses Health Study over a period of 28 years. They found that of the 121,700 women who took part in the study who were between the ages of 30 and 55 in 1976, and used combined hormones for 10 to 14.9 years, had an 88% higher risk of developing breast cancer than women who did not use HRT. Moreover, this risk increased to more than two-fold in women using it up to almost 20 years. And although the risk was comparatively lower for women who used estrogen only, they still had an 22% increased risk for up to 14.9 years and a 43% increased risk for up to 20 years compared to non-users.
Importantly, when the researchers restricted the population to the same that was observed in the Women’s Health Initiative study (i.e. healthy, active postmenopausal women ages 50 to 79 with an intact uterus), they observed a decline in breast cancer risk among women who used estrogen only therapy for less than five years but continued to observe an increased risk among women currently using estrogen fo 15 to 20 years.
Chen emphasizes that the data do not demonstrate an increased risk for dying from, although they continue to study this particular factor for additional clues.
So, what’s the upshot?
Long-term use of any kind of hormone therapy, estrogen alone or in combination with progesterone, significantly increases the risk for developing breast cancer. Is this increased risk worth a decline in hot flashes, night sweats, mood swings and vaginal dryness? Only you can decide.
Read More
Breast cancer: is your environment placing you at risk?
Last week, the Institute of Medicine (IOM) issued a new report on breast cancer and you will want to take note of their recommendations.
Entitled “Breast Cancer and the Environment, a Life Course Approach,” the goal of the undertaking (which was sponsored by Susan G. Komen fo the Cure) was to examine how a woman’s genes interact with her environment outside of her DNA to increase breast cancer risk. For the purposes of this report, environment was defined broadly to encompass all non-inherited factors, including:
- How a woman might grow/develop throughout her lifetime (including body fat, abdominal fat, weight gain as an adult)
- what she eats and drinks (alcohol consumption, use of supplements)
- Physical, chemical and microbial agents encountered (e.g. dyes, BPA, parabens, tobacco smoke, metals, dioxins, pesticides, industrial chemicals)
- her participation in physical activity
- Social and cultural practices
- Any medical treatments or interventions (e.g. combination hormone therapy, oral contraceptives, radiation)
Although research has long focused on the potential interaction between breast cancer and the environment, rarely has it concluded in determining or explaining preventive actions that a woman might take to counteract risk. That’s why I wanted to share some of the key findings on Flashfree.
First a bit of context:
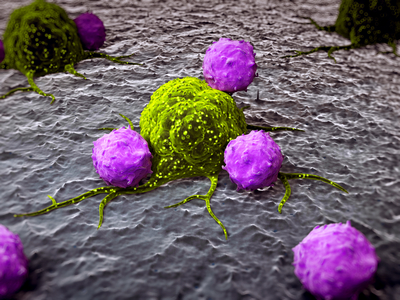
Breast cancer, like many adult cancers is believed to develop as a result of accumulating damage to cells and tissues caused by internal and external factors. According to researchers, timing is everything. In other words, it is possible that a woman’s susceptibility to developing breast cancer increases at key periods during her life; this means when she is exposed to various contributing factors may be important. Overall, girls born in the U.S. have a 12% risk of developing invasive breast cancer sometime during the lives and among White women who are currently age 50 , 24 out of 1,000 can be expected to receive a diagnosis within the next 10 years; this figure declines slightly in women who belong to other ethnicities, including Black women (22 out of 1,000), Asian women (20 out of 1,000) and Hispanic women (17 out of 1,000).
The researchers write that trying to “determine which environmental exposures may influence rates of breast cancer poses substantial challenge,” explaining that how breast cancer develops, where it originates and how it progresses are not entirely clear. They also emphasize that by solely focusing on exposure to these factors during adulthood, it is very possible that they are missing other critical windows earlier in a woman’s lifetime or while she is growing up, that could influence breast cancer risk later in life. Still, even without these missing pieces, they have made some key recommendations that a woman might take to reduce her risk for breast cancer from environmental exposures:
- Avoid inappropriate exposure to medical radiation, especially x rays and gamma rays (i.e. ionizing radiation)
- Avoid combination menopausal hormonal therapy unless medically appropriate (note that not only does this include HRT but also long term use of oral contraceptives)
- Avoid or end active smoking
- Avoid passive tobacco smoke
- Limit or eliminate alcohol consumption
- Maintain or increase physical activity (e.g. increasing specific exercise types or frequency or a combination of the two)
- Maintain weight or reduce overweight or obesity before menopause starts
- Limit workplace and general exposure to chemicals that have been linked to breast cancer
Importantly, some of these steps are not without risk or ramification. For example, avoiding exposure to radiation could result in a loss of clinical information that might be otherwise useful. Likewise, they point out that eliminating alcohol drinking could increase heart disease risk. And, increasing physical activity levels always raises the risk for injury.
The Committee who drafted the IOM report concluded that these steps are only the tip of the iceberg, and that there are still only limited opportunity for evidence-based preventive actions. Moreover, these steps are truly individualistic; what will work for one woman may not work for another. And, any risk reduction may be minimal at best. Still, it is heartening that researchers are starting to tease out how our environment affects our health, if not for us, then for our daughters and granddaughters. Ultimately, we need a better understanding of the relationship between breast cancer risk and environmental factors, of the changes that the breast undergoes through a woman’s lifetime, timing and windows of opportunity. Meanwhile, try to change the course of your life by changing the life of your environment. It can’t hurt.
Read More
Guest Post Roundup: Sex, Generations and A Whole Lotta Love
As we come closer to the year’s end, I’d like to express my gratitude to a few of my colleagues who took the time to publish their thoughts on Flashfree this year. And, althoughI receive a lot of solicitations, there are few that I feel are worthy of your time or your close read. These, on the other hand, rocked my world, not only because of their breadth and finesse but also because of the love behind the words and thoughts.
This is a Roundup that you don’t want to miss.
[Credit: Special and enduring thanks to artist Darryl Willison of whimsicalwest.com. Please visit his site and support his work!]
- Should fatties get a room? Dr. Brian Hughes has lent his fine prose to this blog several times and often writes insightfully about how our society takes advantage of women. When I stumble across something on his blog that screams Flashfree, I reach out and say pretty please. Brian rocks!
- Should I or shouldn’t I? Oncologist, journalist and educator Dr. Elaine Shattner has spent most of her online bandwidth on discerning the facts about breast and other cancers. Let’s face it; there is a lot of information swirling around the Interwebz and when it comes to figuring out what it means, well, the challenge can be daunting. Want to know more? Elaine’s your girl for the 4-11.
- Anti Anti-Aging, Pro Great Glow. Do you want to fight your years? Or fight FOR them? Writer and author D.A. Wolfe dishes up some provocative prose and challenges the inner you. This one’s got “win” written all over it.
- Counterterrorism, women and 9-11. Doesn’t sound like a topic for Flashfree, does it? But my friend Anne Weiskopf shares a poignant piece about what it means to be a woman. And a mother.
- Want to get your groove on? Move. Alexandra Williams, motivational speaker, fitness writer, radio host and inspirateur nails it with a wonderful post on sex, exercise and wellbeing.
- Vagina’s are like self-cleaning ovens. Wait! What?! Yes, gynecologist and sex expert Dr. Jen Gunter makes a guest appearance to shake up the idea that douching is a good idea.
- Have you crossed the Big M finish line? Author Sarah Bowen thought she had. And tells us how she hit the reset button before the race ended.
- On Becoming Bendy. Author Patti Digh is at it again. She’s changing our world, one day at a time. And wow, has she ever changed hers’ this year. Want to be a better you? Bendy. Who said that Gumby didn’t have an alterior motive?
- Are you becoming your mother? When was the last time you looked in the mirror and asked yourself the very question that my friend, motivational speaker and author Cherry Woodburn asks in this post? Are you a generational profiler?