Wednesday Bubble: More on breast tenderness, hormone replacement and breast cancer
More bad news on the hormone replacement front: if you are taking estrogen (conjugated equine estrogen) with progestin (medoxyprogesterone) for menopausal symptoms and experience breast tenderness, you may want to think twice.
Frankly, this news isn’t exactly new. Because back in 2009, UCLA researchers reported similar findings in the Archives of Internal Medicine. These newer data, provided by the same researchers at UCLA’s Jonsson Comprehensive Cancer Center and published online in Breast Cancer Research and Treatment only add to the hormone risk fodder.
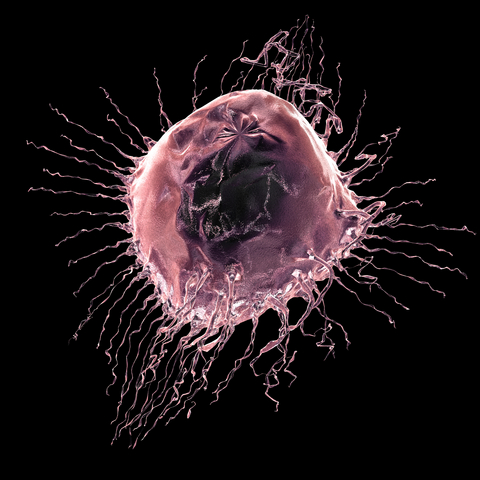
The researchers say that in their research, they’ve consistently run across data that suggest that “estrogen plus progestin compared to estrogen alone, have a more marked effect on breast tissue,” possibly due to more growth, leading to greater density. According to the lead study author, Dr. Carolyn Crandall “higher breast density (has been shown to be) associated with a higher risk of breast cancer,” adding that “in women with extremely dense breasts, the cancer risk can be four to six times higher than for women whose breasts are not dense.”
In this update, Dr. Crandall and her colleagues reviewed data from the Women’s Health Initiative, specifically focusing on reports of new breast tenderness. At the study’s start, almost 12% of women taking estrogen alone or estrogen in combination with progestin reported having breast tenderness. However, by the first year, women in the combination hormone therapy group reporting onset of breast tenderness after starting hormones had a 33% greater risk of developing invasive breast cancer compared with their peers who did not have breast tenderness. And while estrogen alone also increased the risk for developing breast tenderness, the effect was less than that of the combined hormones, especially since it did not lead to an increased breast cancer risk.
So, what to make of these new data? If you are taking HRT and develop breast tenderness, you need to speak to your health practitioner, assess your risks and make a joint decision as to whether or not the benefit of fewer menopausal symptoms is worth the risk of possibly developing an invasive form of breast cancer. And if you are not yet using hormone therapy, you may just want to step back and think twice.
Buyer beware: hormone therapy is a slippery slope with bumps, bruises and perhaps serious disease. Is it worth it? Only you can decide.
Read MoreShaken. Not Stirred.
I have been inspired by my friend Gini Dietrich’s weekly Gin and Topics posts over at Spin Sucks, so much so that I’ve decided to up the ante and bring back a Roundup-like feature to Flashfree (if you’re unfamiliar with the Roundup, think monthly highlight recaps. You can find them here.)
Shaken. Not Stirred is intended to highlight a few choice finds that I believe are worthy of mention in this space. They might not warrant an entire post, but they’ve shaken me up in one way or another to break (or pause, if you will) from our normally scheduled programming and deliver information in a format that is distinct from what you’ve come to expect. In that vein, this feature won’t appear on a regular schedule as I do believe that into every blog should flow a bit of the erratic; after all, that’s what keeps things lively, right?
So, without further ado… I bring you the Shaken. Not Stirred.
Bottom’s up!
- There’s a new kid in town and you may want to get to know him better. So you chat about him online with your other online pals, weigh his pros and cons. And then decide collectively whether or not to befriend him. That’s what the new patient portal Treato is doing. Only this time, the new kid is a medication you might be considering taking for your menopause-related depression and you’re not sure about its side effects. Can you find someone just like you to talk to about it, read/hear their experiences, obtain advice from a medical expert who might be weighing in and then make a more informed decision? Treato is doing just that in one consolidated location. Granted, I’ve not thoroughly vetted the site for accuracy and like any medical information that circulates on the web, ‘whatever is received’ requires vigilance on the part of the user. But I am a huge advocate of leveling the healthcare playing field and patients should be participating in their healthcare. Check it out. And let me know what you think.
- Who knew that weight loss could be so easy? One pair of Zaggora HotPants can help you zap away that unsightly cellulite. How? By incorporating “a comfortable bioceramic material that emits infrared rays to help wearers naturally and efficiently amp up weight-loss regimens. The shorts’ Celu-Lite technology smoothes thighs and other dimple-prone areas by galvanizing the skin’s internal zamboni to promote a deep warming of body tissues and promote lymphatic drainage. This process boosts sweating by up to 80% and aids in eliminating the toxins responsible for cellulite. Gotta give the company props for the term ‘internal zamboni’ but the reality is that nothing has been scientifically proven to rid the body of cellulite.
- Since we are on the topic of do’s and don’ts, why not end this week’s Shaken. Not Stirred with a bit of alcohol-related news? My guess is that many of you have seen the news about drinking and breast cancer and are as confused as I’ve been. My friend Elaine Shattner, over at Medical Lessons Blog, has done an excellent job distilling the facts down to ‘what you need to know,’ much better than I ever could have. Like me, Elaine (who is a trained oncologist, among other things) agrees that women no longer need to be stigmatized by their decisions, writing “Women, in my experience, are generally more vulnerable to the put-downs of others. And so my concern about the BC-alcohol link is that this will, somehow, be used, or have the effect of, making survivors or thrivers or women who haven’t even had breast cancer feel like they’re doing the wrong thing if they go to a party and have a drink. And then they’ll feel badly about themselves.” Do yourselves a favour: read this post.
And if you would, can you do me a favour and weigh in on Shaken. Not Stirred?
Yay, nay or meh?
Read More
On breast cancer screening. Guest post by Dr. Elaine Schattner
Mammography screening. Should you? Or shouldn’t you?
A few weeks ago, I received a letter in the mail from the clinic where I get my mammography. Rather than the expected ‘all is fine,’ the clinic was requesting that I call to schedule another screening due to abnormal findings. Not only was this not the way that I wanted to receive news that something might be wrong, but, I opened the letter at 4 pm on a Friday afternoon, giving me little time to get over the initial shock and then get on the phone to see if I could learn a bit more before the clinic closed for the weekend.
Mammography screening has been in the news quite a bit over the past year, with lines being drawn between experts who say that screening doesn’t save lives and women who want their mammograms regardless of the facts. I happen to fall on the latter side of the aisle and while I suffered a lot of anxiety before I had a second screening, not knowing would have been even worse. (FYI – it turned out fine.)
Recently, my friend Dr. Elaine Schattner, a trained oncologist, hematologist, educator and journalist, wrote about a new review that I believe that every woman should read before deciding whether or not to have a mammogram. It puts some of the controversy into perspective and also provides a much more balanced viewpoint on the risk-benefit ratio. And rather than reinvent the wheel, I asked Elaine if I could re-run the post on Flashfree. Please share it far and wide; it’s important.
With little fanfare, the NEJM published a feature on breast cancer screening in its Sept 15 issue. The article, like other “vignettes” in the Journal, opens with a clinical scenario. This time, it’s a 42 year old woman who is considering first-time mammography.
The author, Dr. Ellen Warner, an oncologist at the University of Toronto, takes opportunity to review updated evidence and recommendations for screening women at average risk for the disease. She outlines the problem:
Worldwide, breast cancer is now the most common cancer diagnosed in women and is the leading cause of deaths from cancer among women, with approximately 1.3 million new cases and an estimated 458,000 deaths reported in 2008.(1)
On screening:
The decision to screen either a particular population or a specific patient for a disease involves weighing benefits against costs. In the case of breast-cancer screening, the most important benefits are a reduction in the risk of death and the number of life-years gained….
She breaks down the data for mammography by age groups:
For women between the ages of 50 to 69 the evidence is clear, she says. For those over 70, there are little data to support breast cancer screening. There’s a consensus that screening isn’t appropriate for women with serious coexisting illnesses and a life expectancy of less than 5–10 years.
For those between the ages of 40–49, Warner challenges the revised 2009 USPSTF recommendationson several counts. She critiques those authors’ weighting of data from the Age trial of 161,000 women, emphasizing the use of an antiquated (single view) mammography technique and flawed statistics. She considers:
…However, this change in remains highly controversial,22, 23 especially because of the greater number of years of life expectancy gained from preventing death from breast cancer in younger women. According to statistical modeling,19 screening initiated at the age of 40 years rather than 50 years would avert one additional death from breast cancer per 1000 women screened, resulting in 33 life-years gained.”
What I like about Warner’s analysis, besides its extreme attention to details in the data, is that she’s not afraid to, at least implicitly, assign value to a procedure that impacts a young person’s life expectancy relative to that of an older person.
She goes on to consider digital mammography and the Digital Imaging Screening Trial (DMIST [NCT00008346]) results. For women under 50 years, digital mammography was significantly more sensitive than film (78% vs. 51%).
The article is long and detailed; I recommend the full read including some helpful tables, with references to the major studies, and charts.
In concluding, the author, who admits receiving grant support from Amersham Health (a GE subsidiary), consulting fees from Bayer and lecture fees from AstraZeneca, returns to the hypothetical patient, and what might be said to a woman in her 40s who lacks an outstanding risk (such as a genetic disposition or strong family history):
…Mammography screening every 2 years will find two out of every three cancers in women her age, reduce her risk of death from breast cancer by 15%. There’s about a 40% chance that further imaging (such as a sonogram) will be recommended, and a 3% chance for biopsy with a benign finding.…
In my opinion (ES) this is key – that the chances of a false positive leading to biopsy are only 3% for a woman in her 40s. If those biopsies are done in the radiology suite with a core needle, every 2 years for women of average risk, the costs of false positives can be minimized.
About the author…Dr. Elaine Schattner is a trained oncologist, hematologist, educator and journalist who writes about medicine. Her views on health care are informed by her experiences as a patient with scoliosis since childhood and other conditions including breast cancer. Elaine is a Clinical Associate Professor of Medicine at Weill Cornell Medical College in New York City where she teaches part-time. Her blog, Medical Lessons, is geared towards dissecting and providing commentary on how healthcare news is comunicated in order to foster learning and help bridge the gap between patients and doctors.
Cancer…it’s still personal
Two years ago, I wrote a post about breast cancer and the fact that it was personal. Very personal. I want to share a portion of that post today and also add a few thoughts. The reason? It’s personal. Again.
Location: Department Store dressing room stall. Circa: late 1960s, early 1970s.
The characters: Me and my mom.
Scene: She is covering herself as she removes her shirt. I notice the scars. Lots of scars….to the side of one breast. I meet her eyes and she meets mine. Then I learn what the term ‘ breast cancer’ means.
My mother was diagnosed with breast cancer when she was 30. Thirty. Even today, less than half of women under the age of 40 are likely to develop breast cancer and the majority of cases are diagnosed after the age of 50. So, imagine the shock. What’s more, imagine the time. 1960… when breast cancer awareness wasn’t at the fore and people didn’t discuss it, when breasts and surrounding muscle were literally hacked off rather than carefully removing the tumor with clean margins, when many men left their wives after they became disfigured.
My dad didn’t leave. And my brother learned about it through a ‘friend’ in school who was teasing him.
I’ve spoken to my mother about her cancer, about the fear of it returning, and about how she feels about not being able to wear sleeveless tops or strengthen/firm those muscles even though she has exercised regularly her entire life. How she felt when my brother came home from school and asked her about it. How she feels now when a friend is diagnosed with cancer. Her answer is always pretty much the same.
But cancer can return. And even though this time it’s not in her breast, it looks like she’s may go down that road…again. And my heart is breaking. Because the fear in the tone of her voice says more than any words can.
She is afraid.
I don’t blame her. I would be afraid too.
Only this time? She’s 80, not 30 and although she’s tough as nails and very, very active, cancer has an insidious nature, sometimes too insidious. And even though in my heart of hearts I believe that she will be fine, I still feel awful about it.
In the past two years, I’ve had two friends who’ve been diagnosed with breast cancer, not for the first but second time. Recently, another close friend developed a very rare form of cancer and despite its severity, emerged in one piece and better than ever. Others in my life are four-, five-time survivors. Hell, even my dad has had bladder cancer since the early 90s. People survive. People move on with their lives. And yet sometimes, we lose people that we love.
Although it may be too early for a Mother’s Day post, it’s never too late to let someone know how you feel about them.
So Mom?
Thank you. The relationship has been a difficult one for most of our lives, threatened by personality and character and actions and words. Often, this road has not been an easy one. But you brought me into this life and I want you to know that despite all, the forks we’ve taken to get to this place have converged and our road is paved with mutual love and respect. I. Love. You. That is all.
And the cancer, I am not certain of the outcome this time. But I am certain of one thing: a mother’s love, and my mother’s love, is one of the most important gifts.
This one’s close to the bone. It’s close to my heart. It’s personal.
Read MoreEstrogen: Worth the risk?
Any regular reader of this blog knows that I am not a fan of hormone replacement therapy (HRT) nor the health risks associated with it. Nevertheless, although I espouse alternative strategies for dealing with menopause, I do feel that sharing news about HRT is important; accurate information leads to informed and shared decisionmaking.
So, do they (i.e. hormones) or don’t they (cause harm)? Undoubtedly, important variables come into play, including current age, how close to menopause hormones are started, current health status, whether or not a woman has had a hysterectomy, smoking history, etc. Also important is whether estrogen is used alone or in combination with progesterone. And yet despite these factors, many medical organizations continue to recommend that HRT be used for the shortest time period possible if at all.
Still, researchers continue to delve into data from the now infamous Women’s Health Initiative Study to tease out the bad, ugly and even the good.
This week, they are reporting on over 7,600 women who had taken estrogen alone for approximately 6 years, had had prior hysterectomies and were followed for an average of 10 years after the trial ended. If you recall, there has been some controversy as to whether or not estrogen alone is safer than combined HRT and actually lowers the risk for breast cancer in particular, which is why these data are particularly intriguing.
The researchers report that age at the time that hormone therapy (in this case, estrogen alone) is started is important. In fact, women who started estrogen therapy in their 50s, an increased risk for stroke and embolism, which appeared while taking estrogen, actually disappeared in the years that followed. Unfortunately, so did protection against hip fracture. Moreover, earlier reports of a decline in breast cancer risk were upheld despite body mass indices. However, the researchers say that this finding in particular, runs contrary to the preponderance of evidence from the majority of observational studies which show that estrogen use increases the risk of breast cancer, especially in lean women and after a long time period of use.
In an accompanying editorial, also in JAMA, the authors point out that more than 80% of women who took estrogen as directed only used it for an average of 3.5 years. Their point is that the results don’t directly address the “balance of risk and benefits associated with longer term estrogen use.” They also point to a larger review of data that show duration is an important factor when it comes to breast cancer risk, especially among lean women. Additionally, they say that tamoxifen, which actually antagonizes estrogen, has been shown to reduce breast cancer by 50%, which has led the International Agency for Research on Cancer to “conclude that unopposed estrogen therapy and combination HRT are carcinogenic.”
Are you confused yet?
Both set of researchers say that the decision to use estrogen or not is one that should be made between a woman and her doctor. Don’t forget: study findings continue to contradict. They add that while “there may still be a role for short-term use of unopposed estrogen for treating some women with menopausal symptoms, this role may be vanishing as existing and emerging data continue to be better understood in terms” of patients.
My thoughts? Err on the side of caution. Always.
Read MoreUp in smoke…smoking and breast cancer in the postmenopausal years
Cigarette smoking is something that appears to keep on giving. And giving. Not only do former smokers find that their habits, even once discarded, might come back to bite them in the hot flash ass and even lead to early menopause, but both active and passive smoking habits are being linked to a increased risk of breast cancer, even 20 years past the expiration date. So, when I was hanging with my bestie behind the fence of my childhood home sucking away at those Kool cigarettes, I guess was I truly making an unconscious choice that is starting to rear its ugly head.
Listen up: don’t smoke.
Okay, enough of the lecture; here are the facts.
Researchers have recently taken a look at the association between smoking and breast cancer risk in almost 80,000 women enrolled in a larger trial (the Women’s Health Initiative Observational Study) that took place in the ’90s. Granted, the study relied upon self-reports, which of course, are subject to some degree of what scientists call “recall bias,” meaning that the findings can be subject to some discrepancies. Nevertheless, after collecting information on smoking (never, former or current), age when started smoking, number of cigarettes smoked daily and number of years that cigarettes were smoked, along with age when quitting, as well as potential exposures to passive smoking (as a child, in the home or at work both formerly and currently), they discovered the following:
- Former smokers had a 9% increased risk of breast cancer and current smokers, a 16% increased risk. These figures were related to smoking intensity and years of smoking.
- If a woman had started smoking before their first full time pregnancy, she had a 21% increased breast cancer risk.
- Among former smokers, time since quitting was relevant, and it took as long as 20 years for a former smoker to return to a risk level that would be considered equal to someone who had never smoked.
- Passive smoking was also a huge factor; in fact women who’s exposure to passive smoke in childhood, at home and at work for 10 years or more had a 32% excess risk of developing breast cancer compared to women who had never been exposed to passive smoke. Note that that the researchers emphasize that this particular association is only suggestive and since this is the first study to so closely examine the link between passive smoking and cancer in postmenopausal women, more data are needed.
So, what about the factors that might have influenced or skewed these findings? Well, the researchers did account for age ethnicity, education, body mass index, physical activity, alcohol use, whether or not women had ever been pregnant or brought a child to term, and history of hormone therapy use. And still, the results remained solid.
The upshot of this is that many of us grew up during a time when smoking was a rite of passage, “cool,” or simply habitual. Many of us quit during our 20s or 30s. Some of us still smoke. However, not only does smoking make those menopausal symptoms ever so much worse, but it’s also risky as hell when it comes to breast cancer.
It’s time to do due diligence. Conduct monthly breast checks. Despite controversy as to their value or lack thereof, make a conscious decision about mammography. Instill healthy habits now, including physical activity, a healthy diet and moderate alcohol intake. We might not be able to take back past habits but we can certainly do all we can to alter current habits.
If I knew then what I know now, I might not have picked up those Marlboro Lights so frequently. Oh well. Payback is certainly a bitch.
Read More