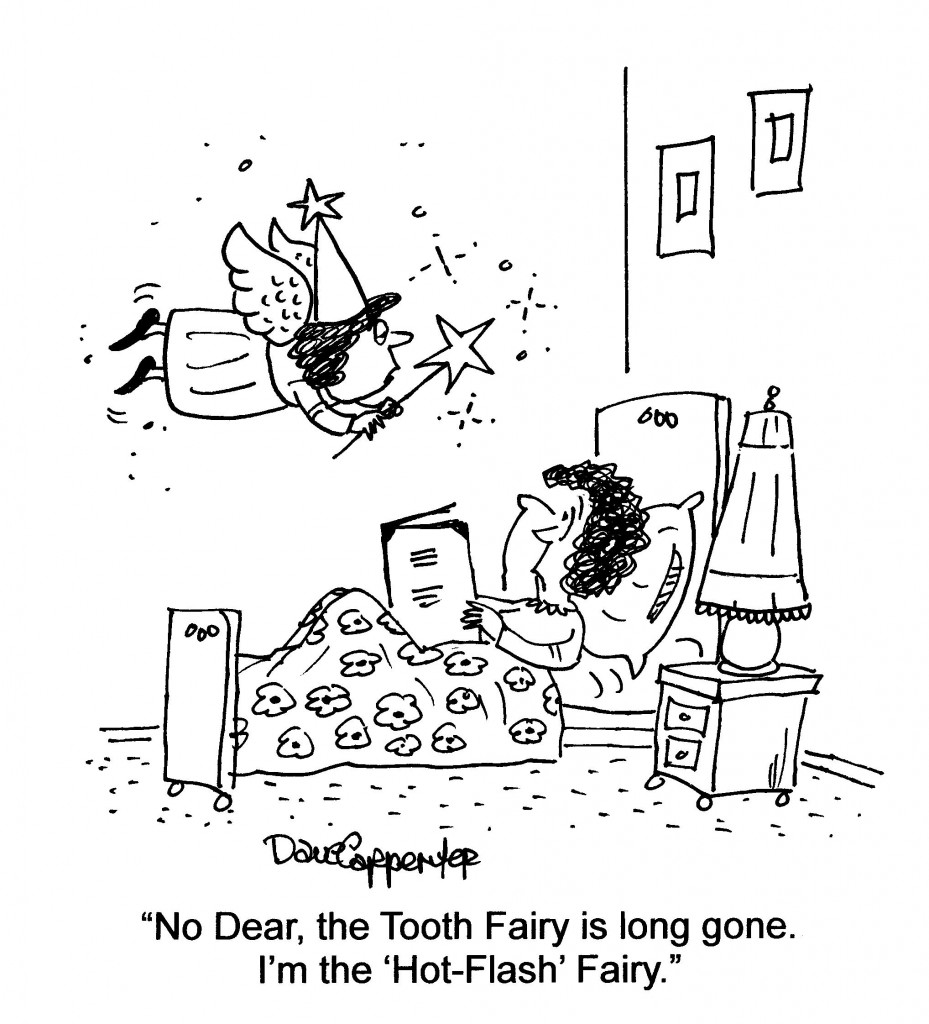
Friday Folly: Long in the tooth…
I was amused to read a post the other day on Facebook about a friend’s child awaiting the Tooth Fairy. And then it hit me: tooth fairy? I’m so long in the tooth that those days are long gone. Now? It’s the Hot Flash Fairy!
Hope you’ll get a few giggles; I did!
Read MoreWednesday Bubble: Evolution?
Do they or don’t they? Inquiring minds want to know!
Tell me what your flashes are like and how they’ve been as you’ve been moving through the ‘pause. Hopefully, we can collectively come up with some effective solutions!
Read MoreFit to be tied: MsFLASH and exercise
Exercise. Does it or doesn’t it? That is, does exercise improve menopausal symptoms? Some studies have shown that it does; and others, like the one I am about to share, shows that it does not.
I am fit to be tied, literally.
Not angry or annoyed but rather, regardless if exercise can improve vasomotor symptoms or not, there is absolutely no doubt that it helps maintain weight, improves overall wellbeing, promotes healthy bones, and may even result in better sleep in midlife. On Wednesday’s post, I shared information about a series of studies called MsFLASH, studies geared towards identifying strategies to alleviate menopausal symptoms and overall health. Today, I ran across one of these trials, published online in Menopause, the goal of which was to clarify the impact of three times weekly aerobic training in women who were in late perimenopause or full menopause reporting frequent and bothersome hot flashes and night sweats.
Exercise/aerobic training can mean a lot 0f things. This time, women who were randomized to 12 weeks of exercise participated in trainer supervised conditioning comprising a treadmill, elliptical or stationary bike for 40 t0 60 minutes each session, with the goal of reaching up to 60% of target heart rate for the first month and up to 70% thereafter (this, along with workload and perceived exertion was measured throughout each session). Likewise, the women had energy expenditure goals relative to their body weight. The other group of women were asked to maintain their usual activity levels but at the end of the study, were offered a one month gym membership or yoga sessions.
While the verdict wasn’t so great for reduction of the frequency and bother of daily hot flashes (both study groups reported declines in hot flash frequency by roughly 2.5% and bother only changed minimally), adhering to training sessions appeared to favourably move the needle for sleep quality and quantity and yielded small improvements in depressive symptoms. Another interesting finding was that race appeared to play a role. Data have shown that African American women actually experience more severe hot flashes than their white peers. And, in this study, while exercise had some impact, albeit minimal, on hot flashes and night sweats, this impact was only seen among white women.
Still unanswered are whether or not small bouts of exercise can positively impact vasomotor symptoms or if individual differences (such as the one that race provides) also play a role. While these questions are being pondered, I’ll leave you where I started: exercise and menopause? Fit to be tied. Don’t give up the activity; it may not help your flashes but it yield a whole lot of benefits beyond cooling the heat that ails.
Read More
NewsFlash: ‘First’ Non-Hormonal Treatment for Hot Flashes – Brisdelle
It’s very important when you see news headlines that you read between the lines.
This came across my mailbox earlier in the week:
Noven Receives FDA Approval for Brisdelle™ (Paroxetine) Capsules, the First Nonhormonal Therapy for Vasomotor Symptoms Associated with Menopause
So, let me explain.
Brisdelle is the first non-hormonal treatment for menopause to receive FDA approval. But, it’s not the first nor the only nonhormonal treatment for vasomotor symptoms; heck, one glance at the tag cloud or the archives and you will see that there are lots.
Claim aside, it’s important to break down the news for you.
Brisdelle is a low-dose form of Paxil, an SSRI antidepressant. Because of its dosage, it is only indicated for treatment of hot flashes and night sweats, and not for depression, obsessive compulsive disorder and anxiety.
This is what I wrote late last year when Noven first presented study findings to the North American Menopause Society:
Paroxetine is not the first antidepressant to be studied in menopausal women and you may recall that I wrote about the use of Lexapro for hot flashes about two years ago. You can find that post here. However, paroxetine is the antidepressant that’s all the buzz right now, since Noven Pharmaceuticals presented two studies last week at the North American Menopause Society annual meeting. Note that it’s been reframed as ‘low-dose non-hormonal therapy for menopausal vasomotor symptoms,’ but ya still gotta call a spade a spade and what it is is an antidepressant.
In one of two studies, 568 women (40+ years of age) who experienced 7 to 8 moderate or severe hot flashes on a daily basis of 50 to 60 on a weekly basis took either 7.5 mg of LDMP or placebo daily over six months. By the end of the first month (and in contrast to the study’s start), women who were taking LDMP experienced 28.9 fewer hot flashes per week (compared to 19 fewer per week for women taking placebo pills). By the third month, this increased by roughly 10 fewer per week in both groups. The severity of the hot flashes also significantly decreased. Safety wise, women taking LDMP reported nausea and bronchitis.
In the complementary study, which lasted for three months, 606 women in the same demographic took the same dose of LDMP or placebo. Decreases in mean number of flashes per week were pretty much on par with the first study (33 compared to 23.5 for placebo) and similarly, a trend towards maintaining and growing benefits were observed. Severity of hot flashes also declined but by the study’s end, were not significantly different than placebo. This time, women who took LDMP most frequently reported dizziness and fatigue.
Dr. James Simon, one of the studies’ investigators and a professor of ob/gyn at GWU School of Medicine claims that symptoms of menopause often go untreated when women are unable or unwilling to take hormone therapy, which is not entirely true. Another investigator — Dr. Andrew Kaunitz from the University of Florida College of Medicine in Jacksonville notes that if LDMP is approved by the FDA, “it could be the first nonhormonal option available for women.” Again, this statement is not entirely true. LDMP has the potential to become the first nonhormonal treatment APPROVED by FDA for vasomotor symptoms in menopausal women. There are other options out there but on the most part, they are not embraced by Western practitioners. Take note: while many Western practitioners will argue until they are blue in the face that alternative strategies have no role, are no better than placebo, and do not have evidenced-based trial data to support their use, they are simply incorrect. An unequivocal statement about every alternative strategy available to wo-man is bad medicine at best and at worst? Sheer ignorance.
Back to LDMP…LDMP appears to effectively diminish hot flashes and sweats but it is not without side effects. And while the dosage is considerably lower than full-strength antidepressants, we don’t have enough information to know if it will ultimately mimic its higher dose partner; the most common side effects reported in these trials are the very same that have been reported with Paxil. Another common side effect of Paxil is the effects on libido and it is a well known fact that as many women go through menopause, they experience declines in sex drive, lubrication and the ability to reach orgasm. In the pivotal studies used to gain approval, about half of the women appeared to have sexual dysfunction; what’s unclear is whether or not the cause was the drug or menopause itself. Another important point that is missing from this story is that back in March, the FDA’s advisory committee on reproductive drugs voted against approval, stating that paroxetine’s effectiveness in reducing hot flashes was underwhelming and not unlike that seen among women taking placebo in clinical studies.
I applaud Noven for its efforts to offer an alternative to HRT, one that has been approved by the FDA. However, the way that communications about this agent are being framed, it appears that the spin masters are working overtime. It’s essential to understand that this treatment is non-hormonal but still a pharmaceutical agent. And while I am a huge proponent of antidepressants for depression, I remain skeptical that they are the best agents for addressing menopausal symptoms. Cost may be an issue – no word on the price point as of yet.
I guess that time will tell.
Read More
Wednesday Bubble: What? When? Memory and Menopause
This past weekend I was discussing the issue of my growing forgetfulness with a friend who, like me, appears to be losing her mind at times. Later that day, upon I landing at a local airport, I realized that I had forgotten where I parked my car only two days earlier. To add insult to injury? I had used a parking app so that I could remember. Only, it took a few minutes before I remembered that I had used the app.
Sound familiar?
Memory lapse is common among women as they transition from premenopause to perimenopause to full menopause, and even appears to cross boundaries and cultures. In the years that I’ve been writing Flashfree, I have run across data linking memory loss to stress, hormones and even a decline in gray brain matter. (If you would like to check out these posts, you can find them here.) Apparently, hot flashes have also been shown to be a significant predictor of so-called forgetfulness. In one study in particular, women were found to experience more memory problems and cognitive issues when they experienced more frequent hot flashes and sweats. Additionally the intensity of those flashes were directly correlated to how long memory issues lasted.
This probable link has been teased out recently in a small (68) pool of midlife women who reported having at least 35 hot flashes a week. Importantly, data were not only based on recall but also, on scientific measures of cognitive functioning (ability to remember words after both short and long delays), menopausal symptoms, sleep and positive and negative moods. With regard to memory in particular, the women were scored on how often they forgot, how serious a failing memory was in those situations, current memory in relation to earlier events in their lives (e.g. 5 years ago, 10 years ago) and the frequency with which they used or didn’t use memory aids. They were also asked to rate their current memory.
One of the most interesting findings was the validation that objective memory performance predicted the magnitude of subjective memory, i.e. the women had an accurate idea of how well or poorly their memory was functioning. What’s more, the higher the numbers of self-reported vasomotor symptoms, the more women recalled having issues in the past, which suggests that women with more vasomotor symptoms — more flashes and sweats — experienced cognitive issues longer than women with fewer symptoms. And, the greater the degree of negative mood — depression, anxiety, hostility — the higher the frequency of forgetting, again, confirming that complaints of memory loss during menopause is not, to coin a phrase, all in your head!
We still lack information on how the relationship between what we believe happens to our memory and what can be measured or confirmed changes as we age or across different menopausal stages. However, the data lend credence to claims that memory is changing during menopause, especially in terms of performance on tasks, and that our mood can influence how well we comprehend or judge the severity and seriousness of those lapses.
Feel like you are losing your mind at times? If you are in the throes of the ‘pause, this feeling may not be going away any time soon.
Read More