Who put the ‘men’ in menopause? Part deux.
Bob LeDrew, that’s who!
There’s some changes going on and it’s not of the menopausal kind. Starting next week, in fact, my friend and sometimes partner in Words with Friends is joining FlashFree with his new monthly column: Guyside.
Yup, Bob’s going to bring a bit more y into our x’s, testosterone into the estrogen and hopefully, bridge some of the communication gaps that pervade this thing we call midlife.
The few glimpses that I’ve been afforded not only excite the hell out of me but, I know that this new twist is going to shake up this space in ways that I could only dream of previously.
Stay tuned. Menopause has got a ‘brand new bag’ (sorry, my friend!) and his name is Bob!
p.s. If you didn’t catch his guest post last month, Falling into the trips of masculine invulnerability, you are missing out. Check it now!
Read MoreStill feeling like a shadow of your former self?
Must be “Low T,” right?
Low T is a global problem of epic proportions. In fact, UK researchers are reporting that testosterone prescribing has reached epidemic proportions, with an increase in prescriptions by almost 90% between the years 2001 and 2010. Moreover, the majority of these prescriptions have not been for an established hypogonadism (a decline in the functional ability of the testes to produce ample amounts of testosterone. This can lead to erectile dysfunction, low libido and a low sex drive. Aside from sexual dysfunction, hypogonadism can also cause depression, lethargy and fatigue. And yet, the most recent statistics from the Urology Care Foundation suggest that low T is a problem mostly affecting men 60 and above. In the UK study, only 6.3% of men had definite hypogonadism. So, what gives?
Money.
A few years ago, the pharmaceutical industry jumped on the male menopause wagon and the current campaign is a doozie. The condition? Low T, which is better known as low testosterone, andropause or the commonly used misnomer, “male menopause.” In fact, you can take a simple quiz to learn if you have Low T and if you need to speak to your doctor.
I’ve written about male menopause and have also directed readers to data that shows that it may not be all that it’s cracked up to be. Is it irritable male syndrome? Or is it another marketing tool to sell drugs to unsuspecting men who are aging and losing their virility?
Truly, if you are feeling like a shadow of your former self, there may be other things at play than testosterone. You might want to speak to your healthcare practitioner before jumping on the Low T wagon. Too much testosterone can lead to heart disease and negatively affect the prostate gland.
The medical community remains unconvinced about the condition and the need to treat it. In fact, that might be why, in 2011, University of Pennsylvania researchers started putting it to the test with the T Trial, which may solve this question once and for all.
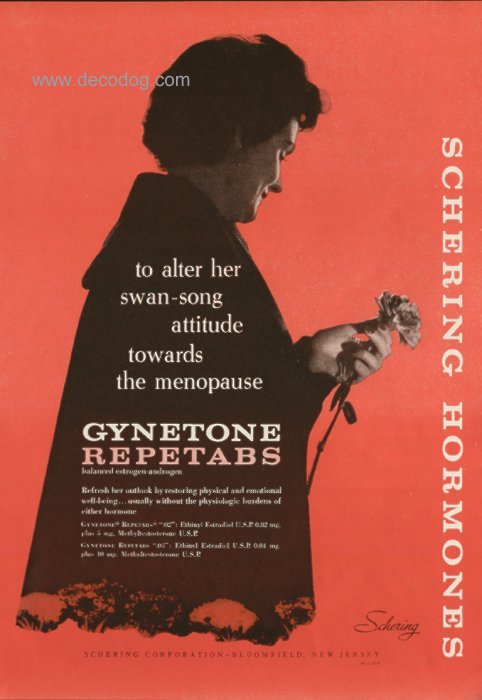
Read MoreWednesday Bubble: Refresh your outlook. With Gynetone…
[Image: http://www.decodog.com/inven/medical.html. All trademark rights reserved]
Gynetone. Sounds like a band, right? But this band won’t be music to your ears.
Gynetone Repetabs, an early form of hormone replacement therapy evidently was formulated to refresh more than your outlook. And the tagline “without the “physiologic borders of either hormone” had a whole lotta subtext.
Interestingly, this nifty hormone replacement pill contained ethinylestradiol (the first orally, active semi-synthetic estrogen used) and methyltestosterone of all things. Methyltestosterone is an anabolic steroid used to treat testosterone deficiency in men. It also stimulates aggression.
Alter your attitude? Sure, we’ll just give you a dose of aggression and your ‘swan song’ outlook will turn you into the Amazing Hulk. Your new song? Momma gonna knock you out?!
Read More
Wednesday Bubble: Hairs and acne and heart/breast conditions. Oh my!
 Back in 2008, I wrote about Intrinsa, a testosterone patch that was tested in a study of 841 postmenopausal not currently on hormone replacement therapy to evaluate effects in terms of improving sexual desire. The results, which were published in the New England Journal of Medicine, showed that compared to a dummy patch, use of low or high dose Intrinsa was associated with significant increases in sexual desire and a decline in sexual distress. Overall, the higher dose patch led to modest improvements in sexual function. In other words, wearing a patch was significantly better than using nothing at all but not life-shattering in terms of improving sexual function.
Back in 2008, I wrote about Intrinsa, a testosterone patch that was tested in a study of 841 postmenopausal not currently on hormone replacement therapy to evaluate effects in terms of improving sexual desire. The results, which were published in the New England Journal of Medicine, showed that compared to a dummy patch, use of low or high dose Intrinsa was associated with significant increases in sexual desire and a decline in sexual distress. Overall, the higher dose patch led to modest improvements in sexual function. In other words, wearing a patch was significantly better than using nothing at all but not life-shattering in terms of improving sexual function.
Once I delved further into androgens and women, I learned that while it has been suggested that local circulating levels of androgens are associated with low sexual desire and sexual dysfunction, the data are contradictory. Moreover, in a fairly recent scientific review, researchers say that no single androgen predicts which women will have sexual dysfunction, making it even harder to address, right? What’s more, they also note that laboratory studies have only limited value and aren’t routinely recommended.
Still, researchers continue to evaluate the role (if any) of testosterone treatment in female sexual dysfunction; the latest study on the dockets is the BLISS trial, which is examining the long-term effects (i.e. 60 months) of a low dose testosterone gel — LibiGel — in natural and surgically-induced menopausal women. This trial was requested by the FDA to insure that testosterone can be safely used without specifically causing heart disease or breast cancer ( note that the focus of this study is specifically on the risk for heart-related events, including death, nonfatal heart attack, nonfatal stroke, chest pain, and clotting events and death, and breast cancer). Importantly, researchers still don’t know much about the safety of long-term testosterone in either men or women, although it is a known precursor of estradiol, a hormone that has been shown to stimulate breast tissue. With regard to heart issues, women with polycystic ovarian syndrome have elevated blood testosterone levels and are at risk for obesity, high blood pressure and insulin resistance, all signs of heart disease.
Although questions about heart disease and breast cancer remain unanswered, experts have evaluated numerous formulations of androgens like testosterone, e.g. patches, oral tablets, implants and injections, and say that the major side effects are unwanted hair growth and acne. Both are related to dose and how long treatment lasts, and disappear once treatment is stopped. And while rates of hair growth are definitely lower for patches in general (as few as 7% to as high as 23%), as many as 36% of women who use oral testosterone have unwanted hair growth. Among those receiving implants, pellets or injections the number is also high: 20%.
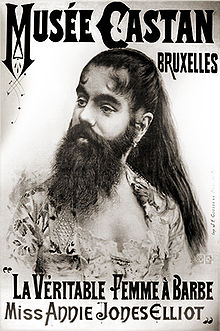
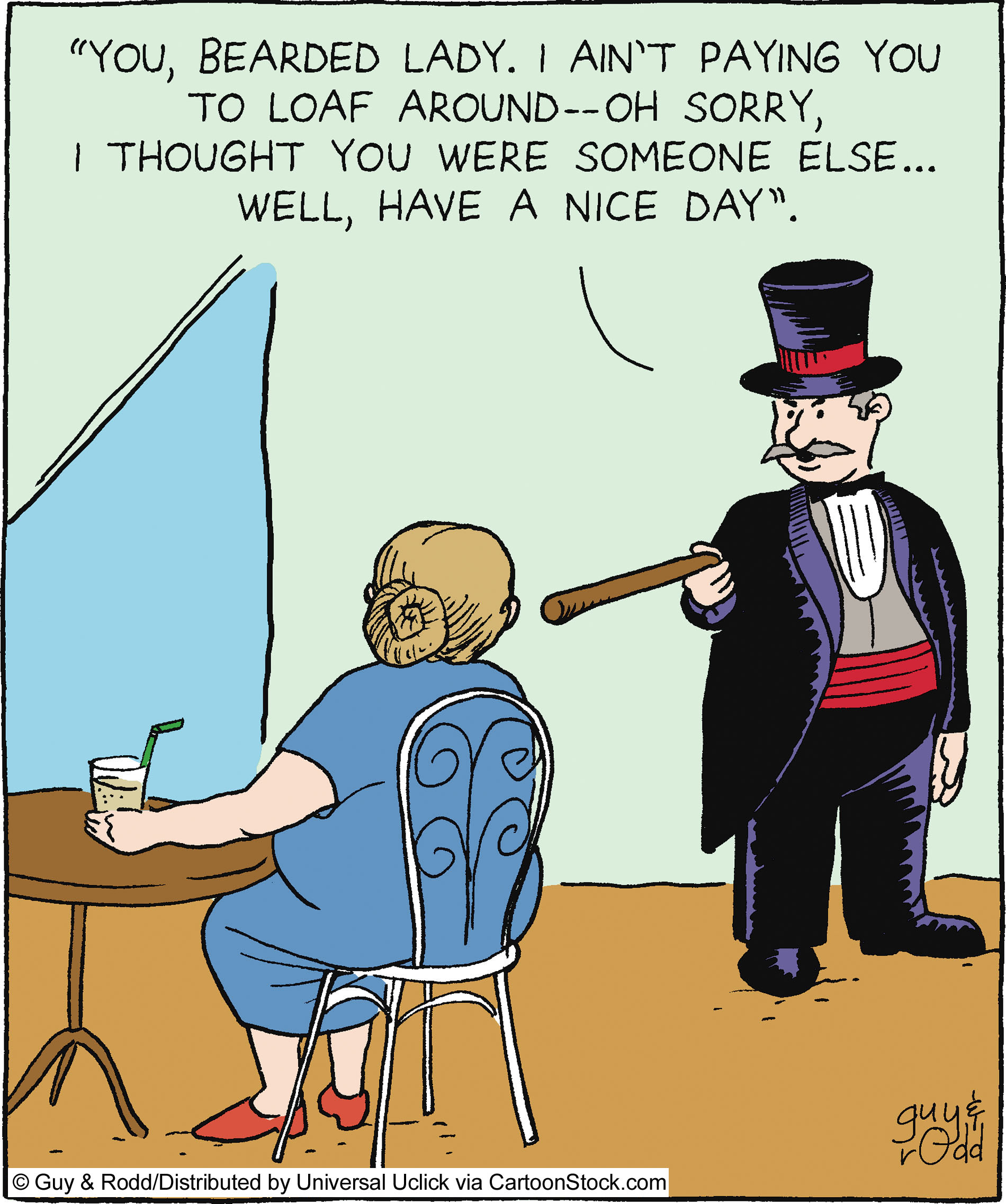
Let’s face it; the trouble is testosterone is that it may only address a miniscule amount of factors affecting a woman’s libido and in literally leave a trail in its place, not only of unwanted hair and blemishes, but perhaps more serious issues. What do you think? Is testosterone a hairy proposition? Should the bearded lady shave before her handler pushes more patches and gel?
Stay tuned…
Read More
Hairy kiri…sexual desire and hairs on your chinny chin chin
Yes, I am taking poetic license with the Japanese term “Hara-Kiri” which literally means to cut or slice the stomach. This phrase has been hijacked by slangers who refer to it as ‘hari kari,’ to off oneself or commit suicide.
I propose that using testosterone in hopes of improving sexual desire is a great way to cut off one’s wellbeing and sense of self Chi, leaving hairs on the chinny chin chin and other undesirable locations.
Hairy kiri? You bet!
Back in 2008, I wrote about Intrinsa, a testosterone patch that was tested in a study of 841 postmenopausal not currently on hormone replacement therapy to test its effects on sexual desire after about a half a year’s use. The results, which were published in the New England Journal of Medicine, showed that compared to a dummy patch, using low or high dose Intrinsa was associated with significant increases in sexual desire and a decline in sexual distress. Overall, the higher dose patch led to modest improvements in sexual function. In other words, wearing a patch was significantly better than using nothing at all but not life-shattering in terms of improving sexual function. However, the caveat was unwanted hair growth, which occurred in about a third of women using the higher dose patch and in about 23% of women using the lower dose.
Once I delved further into androgens and women, I learned that while it has been suggested that local circulating levels of androgens are associated with low sexual desire and sexual dysfunction, the data are contradictory. Moreover, in a fairly recent scientific review, researchers say that no single androgen predicts which women will have sexual dysfunction, making it even harder to address, right? What’s more, they also note that laboratory studies have only limited value and aren’t routinely recommended.
Looking more closely at different formulations of androgens like testosterone, e.g. patches, oral tablets, implants and injections, experts have found that the major side effects are unwanted hair growth and acne. Both are related to dose and how long treatment lasts, and disappear once treatment is stopped. And while rates of hair growth are definitely lower for patches in general (as few as 7% to as high as 23%), as many as 36% of women who use oral testosterone have unwanted hair growth. Among those receiving implants, pellets or injections the number is also high: 20%.
Let’s face it; the trouble is testosterone is that it may only address a miniscule amount of factors affecting a woman’s libido and in literally leave a trail in its place. Don’t know about you but I think it’s a hairy kiri proposition. A few more notches on the desire scale and a few more hairs in your chin, on your chest and lord knows where else.
Committing hairy kiri ain’t for sissies; that’s for sure!
Read More