Midlife mishap: blurring the boundaries between work and home
Telecommuting is the new black, right?
Not so fast.
Researchers say that while telecommuting (i.e. working regularly but not exclusively at home) has gained traction in the American workplace, the foothold remains elusive and the proportion of workers with flexible work options has been essentially flat over the past decade and a half. Additionally, the number of hours that workers actually telecommute on a weekly basis is less than one full day, a mere six hours. Although the reasons for this are numerous, it appears that managers remain reluctant to relinquish supervisory control, even though on average, telecommuters work harder and longer than their colleagues who are tied to their office chairs.
Do the math: Fewer telecommuting hours still equates to longer working hours.
What this brings to mind is the potential impact that telecommuting has on our lives outside of work, especially when work takes place at home? And how does this impact in turn, affect stress, which of course, has been linked to worsening of menopausal symptoms such as weight gain, hot flashes and depression?
I have been working at home for 20 years now, having started a business in 1992. While I am not a telecommuter, I am very aware of the black hole that one can fall into and how that has affected my ability to shut it down after a certain time of day. This ability has grown more difficult the more connected the world is and I find that I am consistently interrupted by clients during gym workouts, breaks, early morning coffee reentries and late day ratchet down.
Data demonstrate that my experience is often the norm and not the exception.
Let’s take a look at what the research shows. Analyzing trends from two national data sources — the National Longitudinal Survey of Youth 1979 Panel and the U.S. Census Bureau’s Current Population Study — Sociology Professors Mary Noonen and Jennifer Glass from the University of Texas at Austin learned that while the number of weekly telecommuting hours is relatively modest (just 6 hours, per above), most of the 30% of respondents who work from home add at least five to seven hours to their work week. In fact, 50% to 67% of telecommuting hours reported in these surveys push work hours past the 40 hour workweek model and are essentially overtime work. Just think: if you feel that you are already pushed to the brim in the office and volley for work at home hours, you may actually be relocating hours but not eliminating them. Moreover, your employer may be raising his or her expectations not only of what you deliver but when, including evenings and weekends.
Study findings also show that there is a misconception that telecommuting is more prevalent among parents with dependent children. In fact, parents are not likelier than the general population to work from home; rather authority and status in the workplace appear to drive telecommuting hours.
The researchers note that “telecommuting is intrinsically linked to information technologies that facilitate 24/7 communication between clients, coworkers and supervisors [thereby] potentially increasing the penetration of work tasks into home time.” A 2008 Pew Study supports this contention, demonstrating that the majority of ‘wired workers’ use technology to perform work tasks, even while sick or on vacation.
The perils run deep when the boundaries become blurry between work and home. Moreover, over wired means overload, and the ability to shut off our brains becomes increasingly difficult. Adrenal fatigue may set in, where after prolonged periods of cortisol production overdrive, the adrenal glands can no longer keep up with outside stressors and the body’s demand to handle stress and protect the immune system. In turn, the ability to handle life stressors declines.
Do blurred boundaries yield diminishing returns, midlife mishaps, a mishmash of expectations?
What do you think?
Read More
Wednesday Bubble: Relax, just do it.
You think that hormones are the only solution to hot flashes?
Think again!
This is not the first time that I have reported that the mind-body connection is an important key to menopausal symptoms. Moreover, it probably won’t be the last. In fact, in a second study published within the past 18 months in Menopause journal, researchers are again moving away from hormones and moving towards applied relaxation. (A related study topic-wise can be found here.)
This time, Swedish researchers assigned 60 women in menopause to either ten sessions of group therapy combined with relaxation or to no intervention for three months. All of the women had been experiencing moderate to severe hot flashes at least 50 times a week. During the 10 group therapy relaxation sessions, the women were taught to methodically move through the body’s muscle groups and use breathing techniques to systematically relax each group. They were then provided with exercises to practice daily at home, with the the goal being to learn the relaxation method and self-manage their symptoms. During this period, all participants kept a regular hot flash diary and filled out a quality of life survey on three different occasions. They also provided the researchers with a sample of their saliva.
The findings? Women practicing daily relaxation and engaging in regular coaching sessions actually reduced their daily hot flash count from an average of 9.1 to 4.4 a day; that’s about a 50% reduction. In the group of women who had no interventions, a reduction in daily hot flashes was also observed but on average, these women experienced less than two fewer flashes a day; this is likely the result of what researchers consider a ‘placebo effect.’
More importantly, benefits of relaxation remained for at least three months after the study ended and the final therapy sessions. The women who practiced relaxation also reported improvements in overall wellbeing and quality of life, including sleep and memory. What’s more, saliva testing showed reductions in cortisol; as I’ve written previously, stress leads to cortisol release and ups the hot flashes ratio. Once that cycle starts, who knows how long the endless loop plays out?!
Time to stop the loop? Forget the drugs. Breathe deeply, exhale and repeat. Just do it.
Read More
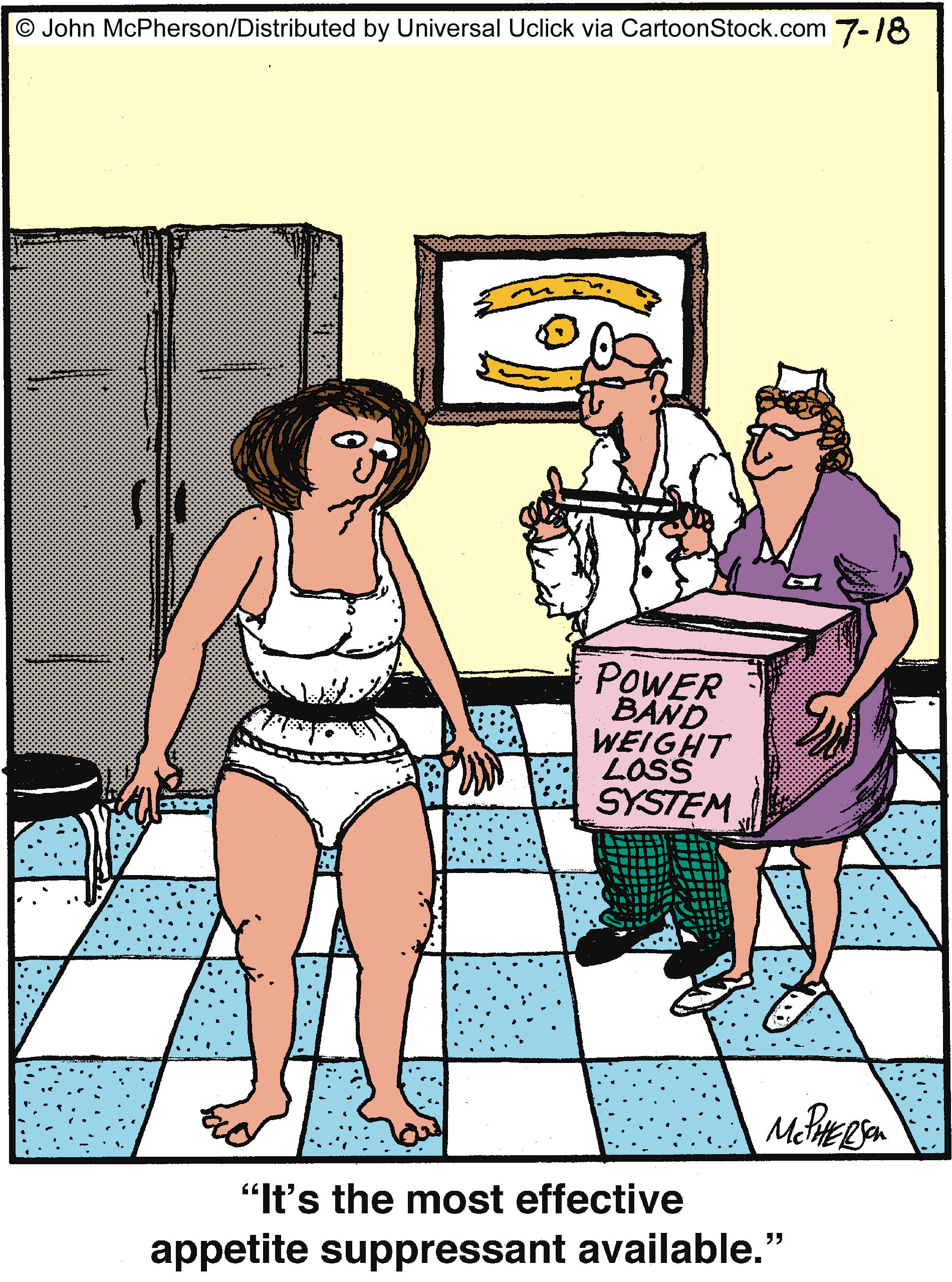
Battle of the midlife bulge: diet+gender=
I am on a roll! On a roll around my midsection, that is.
Ever wonder why women may be likelier than men to gain fat in their abdominal area, especially as they go through menopause? Yup, we’ve talked lots on Flashfree about estrogen, exercise and even stress and the release of cortisol and how they affect that growing tummy donut. However, researchers are now adding another factor into the mix that may occur especially in women: a high-fat diet. Mind you, this particular study, which is published online in Diabetes journal, was conducted in mice so it’s way too early to comment on how the findings affect actual humans. But what it does imply is that diet might not be the only factor at play and in women, genetics and gender play an equally important role.
Researchers say that when female mice were fed a high fat diet, it triggered the production of an enzyme (called aldehyde dehydrogenase 1) that produce a hormone — retinoic acid — that boosts the formation of fat around the abdomen. Let’s step back; high fat diet leads to enzyme, leads to retinoic acid leads to belly fat. Got it?
Interestingly, not only is this enzyme activated at nine times the level in female versus male mice, but when removed, this domino effect disappears. What’s more? Estrogen can suppress the enzyme so when it starts to decline, women become more prone to developing that midsection bulge.
The culprit here is vitamin A and how the female body processes it. One of the functions of vitamin A is to produce a molecule that supports how the body burns both fat for energy and retinoic acid. Evidently, high fat diets can directly shut down the fat burning molecule and the domino effect begins, resulting in the midlife bulge many of us have come to know so well.
The good news is that on a regular diet, female mice barely produced retinoic acid, meaning the simple solution for women may be to stay away from high fat meals as much as possible.
If you can’t burn it, and you can’t rely on estrogen to keep the fire going (or take it away -ironic, right?!), then take some steps and do it yourself. D is for diet. F is for female. The endgoal? Do the math.
Read MoreStress eating? Spare Tummy Tire? Try a little mindfulness…
Mindfulness. It keeps popping up in different areas of health. Last time I posted about mindfulness training, it was within the context of hot flashes and how training your mind to reduce stress can influence how hot flashes are experienced. But what about stress eating?
Many women (and men) turn to emotional eating when they are stressed. And unfortunately, when it comes to weight gain, many of the most serious health affects of excess weight tend to be linked to that roll around the tummy area. In fact, abdominal (or visceral) obesity produces inflammation in the body that can increase the risk for diabetes and heart disease. In women in particular, who may be prone to weight gain in their abdominal area due in part to hormone fluctuations, it’s a double-edged sword. Add the fact that chronic stress increases levels of cortisol, which in turn, mobilizes the migration of fat cells to the midsection, and well, it’s a disaster in the waiting.
As I have written previously, cortisol is a hormone that is secreted by the adrenal glands. Its primary role in the body is to regulate energy (by producing blood sugar or metabolizing carbohydrates, protein and fats) and mobilize it to areas where is it most needed so, cortisol levels tend to peak in the early morning and then gradually decline throughout the day. Research has shown, however, that women have higher cortisol levels than men, and that certain women –especially those with greater amounts of abdominal fat — may be reacting to a large disruption in the release of cortisol that causes a greater than normal difference between morning and evening levels of the hormone. This disruption is believed to be related, at least in part, to exposure to prolonged physical and mental stress. This psychological component is huge, because it tends to trigger the desire to consumption of food that is high in fat and/or sugar, which also tends to promote abdominal weight gain.
How do you break the cycle?
Researchers are now saying that mindfulness may be an important strategy to beat the bulge and the stress. In fact, whey they looked at the effects of a program that focused on interrupting habitual thoughts, emotions and behaviors, that is exactly what they found.
In this small exercise, 24 overweight and obese women not yet in menopause learned to use guided meditation as a way to introduce mindful eating (i.e. paying attention to their physical sensations of hunger, stomach fullness, taste satisfaction and food cravings). They were also taught to be more aware of emotional eating triggers and negative emotions as well as to be more loving and accepting of both themselves. Over nine weeks, they were able to share their challenges, concerns and experiences and then learned new meditations to overcome what they felt were roadblocks in their progress. During the same four week period, 23 women were placed on a waiting list for comparison purposes.
Regularly engaging in mindfulness training set these women off on the right foot upon awakening and in fact, lowered their cortisol levels in the early am hours. What’s more, women who reported having the greatest improvements in their response to stress and emotional eating triggers tended to have the largest reductions in abdominal fat. Additionally, reductions in waking cortisol levels were related to reductions in abdominal fat as well.
Mind you, the women in this particular study were premenopausal, namely because the researchers say that hormonal declines naturally lead to deposits of fat in the midsection. However, if psychological stress compounds weight gain in this area as much as it affects overall wellbeing and menopausal symptoms, it might be worthwhile considering if incorporating ‘a little mindfulness’ into one’s life could help shift fat away from the abdomen as well. It’s an interesting idea and definitely worth exploring…especially as we move into what many regard to be the most stressful and eating laden season of the year: the holidays!
Try a little mindfulness. Not only can it benefit your brain but your tummy might reap the benefits as well.
Read MoreNeedles and symptoms and a pathway, revealed…more on acupuncture
Click on acupuncture in the tag cloud and you’ll know that I’ve spent a number of years examining and sharing information about important studies on this blog. In some, acupuncture has been shown to alleviate vasomotor symptoms like hot flashes and night sweats, and in others, acupuncture appears to be no better than placebo or sham needles that are placed on accurate points but not actually inserted into the skin. However, I’ve also long argued that by slightly changing the way that we conduct scientific studies in the West and allowing for individualization, observed benefits might be different. Indeed, that’s exactly what researchers have seen with ACUFLASH and you can read more about that trial here.
Less clear that whether or not acupuncture can help symptoms (for the record, I am biased and I believe that over time it can), is HOW it works. The centuries old Chinese medicine paradigm is never so apparent than with acupuncture and although I am not sure why we need to know the ‘how,’ I am fairly certain that until it is revealed, there will be a lot of researchers and health practitioners questioning its validity or utility.
So, this brings me to a wonderful pilot study in the online version of Menopause, exploring that very question: how does acupuncture work on vasomotor symptoms?
In this small trial, 33 perimenopausal and postmenopausal received traditional acupuncture, sham acupuncture or nothing over a period of 12 weeks. The active groups received three treatments per week and all the women reported having at least 7 hot flashes a day. But there’s the rub: the researchers also looked at how traditional acupuncture affected the hypothalamic-pituitary axis (HPA), the part of the body that comprises the hypothalamus and pituitary and adrenal glands, controls digestion, our immune system, mood and emotions, sexuality, and how energy is used and stored. Moreover, this part of the body reacts quite negatively to stress by releasing a hormone known as cortisol. Not surprisingly, women who have very severe vasomotor symptoms tend to produce high levels of cortisol.
What did they learn?
- Most of the benefits, (e.g. reductions in hot flashes) occurred by week five and; hot flash severity and frequency declined by 86% and 78%, respectively in both the real acupuncture and sham acupuncture groups. But while the sham acupuncture group didn’t continue to improve, the real acupuncture group did.
- Likewise, anxiety and depression improved in both of these groups, as did sleep scores.
And the “how?”
It appears, at least from this small study, that acupuncture positively affected levels of cortisol and DHEA, the major steroid secreted by the adrenal glands that affects none other than the body’s production of estrogen. Consequently, if acupuncture helps to control the HPA, and HPA affects vasomotor symptoms, then perhaps scientists have the first clue as to why acupuncture may help certain menopausal symptoms. It also opens up an entirely new avenue for novel strategies to control them.
The bottom line is that there is hope and a new direction that researchers will ideally follow. Ultimately, acupuncture may prove to be even more effective than pharmaceutical strategies for menopausal symptoms and definitely, much safer.
The jury’s still out but it seems a helluva closer to a verdict.
Read More