Friday Folly: Mind-Body Medicine
Personally, I am a huge fan of mind-body medicine.
You?
Have a beautiful weekend!
Read More
The present of being present: cortisol and mindfulness meditation
Sometimes things are just timely. Like this post, which I am bringing back today for your consideration.
Happy Friday, folks! Wishing you a stress free weekend!
It seems that I write about stress a lot on FlashFree. Perhaps that is because like many, my life — namely my work — can be very stressful from time to time. However, according to the American Psychological Association, I’m not alone; most Americans suffer from moderate to high stress and the problem does not appear to be going away. Moreover? Work issues are the primary stressors in 77% of people.
From a midlife perspective, stress and its related hormone, cortisol, can cause a lot of health-related problems. In fact, not only does cortisol promote a fat dump in the midsection, but experts say that overexposure to cortisol and other stress hormones has a cumulative affect, leading to heart disease, sleep issues, digestive issues, obesity, depression and worsening of skin conditions. It’s critical to counter stress’ negative effects before they take their toll and start to do permanent damage. One important strategy to achieve a better balance is meditation.
Fortunately, a team of researchers at UC Davis’ Center for Mind and Brain are devoting time to studying psychological and physiological processes in order to explain the benefits of meditation. The framework for this effort is the Shamatha Project, which is apparently the most comprehensive meditation study ever undertaken. Most importantly, this scientific twist on a centuries old practice may ultimately elevate meditation’s place in Western medicine.
To better understand the effects of meditation on stress, the research team recently took 60 people (between the ages of 22 and 69) who had some prior experience with meditation, measured cortisol and body mass index and their current degree of ‘mindfulness,*’ and then randomly assigned them to a three month meditation retreat or a waiting list. Those on the waiting list participated in the same, three-month retreat at a later date. (*Participants completed a mindfulness questionnaire that measured the degree that these people directed their cognitive resources to sensory experiences and how often they drifted, as well as their ability to let go of distressing thoughts.)
At the retreat, the group met two times a day for one hour, guided sessions and the rest of the time (around 6 hours) practiced solo meditation in 20 to 30 minute increments. Meditation practices were focused on mindful breathing and relaxation and promoted compassion and kindness toward others. Overall, the emphasis was on present awareness rather than meandering into the future of ‘what if’s.’ During the middle of the retreat, all were encouraged to enter into silence for a period of about four weeks. Aside from scheduled meals and group meditations, everyone was on their own to decide sole meditation, exercise and free time.
Did learning how to direct and focus attention away from uncontrolled, ruminating thoughts and worry and toward a chosen target reduce cortisol levels? The researchers say that they found a correlation between a high score for mindfulness and a low score in cortisol, both before and after the retreat. The results were greatest for participants who were able to achieve the greatest increases in mindfulness, that is, the more that they reported directing their thoughts to the present/immediate experience, the lower their resting cortisol levels were. Participants also experienced large improvements in overall wellbeing, daily mood and emotional functioning.
While the findings do not prove cause and effect, they do suggest that changing the mind paradigm to focus on the now rather than the future may ultimately help to reduce our tendency to think about the past or worry about the future and in turn, counter excessive cortisol release.
Tonya Jacobs, a postdoctoral researcher and the study’s lead author, explains that “the idea that we can train our minds in a way that fosters healthy mental habits and that these habits may be reflected in mind-body relations is not news; it’s been around for centuries. But, accumulating evidence might help the idea — that the present is the best present we can give ourselves — be better integrated into Western mentalities and health practices.
Mindful meditation may ultimately prove to be one of our strongest defenses against stress and its companion, cortisol!
Read MoreNewsflash: Yoga and hot flashes
When it comes to alternative strategies for managing hot flashes, where do you turn? I’ve been writing about alternatives for five years now and the only thing I am fairly certain of is that what works for one woman doesn’t necessarily work for the next. Consider the management of menopausal symptoms similar to the management of any condition: the best treatment is always individualized.
Still, mind-body practices tend to rise to fore and evidence continues to accumulate supporting their value and usefulness. This is especially true of meditation, and of yoga.
The latest news on yoga comes from the online edition of Menopause journal and researchers are saying that integral yoga practice may help to reduce hot flash frequency among some women.
Integral yoga integrates the various branches of yoga and focuses on a whole body approach with the goal of transforming the entire being. Experts say that it is especially well suited to hot flashes because it emphasizes stress reduction and decreasing the likelihood of becoming overheated.
To evaluate its usefulness in a more scientific setting, researchers asked a small group of women in perimenopause who reported at least four hot flashes a day to participate in 10 weekly, 90-minutes integral yoga classes comprising breathing, centering medication, physical postures and deep relaxation, or health and wellness classes on different topics relevant to menopause and midlife women’s health or no interventions at all. All had the option to join classes at any time, and were required to fill out diaries about their flashes.
The findings? The researchers say that even after controlling for a potential placebo effect, both the yoga and health and wellness groups tended to follow a similar pattern and a similar significant decline in hot flash frequency. Women in these groups reported an estimated 66% (yoga) and 63% (health/wellness) decrease in the frequency of their hot flashes. And, while the effectiveness of yoga to lower hot flash frequency was not considerably different than that of the health/wellness education classes, the inclusion of the two behavioral interventions may perhaps capture naysayers’ attention; most studies only include on behavioral intervention and having two helps to temper bias.
We need more studies like this one to tease out the benefits of behavioral interventions. The good news is that the information is there for those who look deeply enough.
Read MoreWednesday Bubble: No mystique, just perseverance
 Time for another menopause downer…followed by some good news! First the downer: declining levels of estrogen during menopause tend to reinforce a decline in the body’s ability to naturally metabolize blood fats and its ability to fight off the ravages of oxygen-free radicals, you know, free roaming oxygen ions that can wreak havoc on the immune system. The result is often an upsurge in heart and other metabolic diseases. You can read more about those conditions here.
Time for another menopause downer…followed by some good news! First the downer: declining levels of estrogen during menopause tend to reinforce a decline in the body’s ability to naturally metabolize blood fats and its ability to fight off the ravages of oxygen-free radicals, you know, free roaming oxygen ions that can wreak havoc on the immune system. The result is often an upsurge in heart and other metabolic diseases. You can read more about those conditions here.
Okay, so the good news: it appears that Tai Chi training may help increase the body’s antioxidant defenses in both pre- and post-menopausal women! In fact, in a study published a few years ago in the Journal of Aging Research, investigators noted a marked change in antioxidant markers normally related to aerobic exercise, as well as a decline in a marker for heart disease risk.
For those of you unfamiliar with Tai Chi, it is an ancient Chinese martial art form that combines breathing with smooth, gentle postures. It may look fairly tame, however, having studied Tai Chi for a short period of time, I can assure you that it’s damn hard. Moreover, despite appearances, it is a weight-bearing exercise that not only strengthens muscles but also is on par with moderate intensity aerobic exercise. It has also been shown to improve mobility, flexibility and balance, improve sleep and overall wellbeing, and even enhance the circulation of blood through the smallest of blood vessels.
I’ve written about the effect of breathing on stress and the body’s stress markers. However, it appears that when Tai Chi is combined with slow and deep breathing exercise (i.e. 6 breaths per minutes) overall benefits are boosted. Indeed, two, 75-minute Tai Chi sessions a week combined with two hours of at home practice appeared to do just what the doctor ordered. These sessions involved 10 min of warm up/stretching, 60 minutes of Tai Chi (45 minutes 18-posture Tai Chi and 15 min Tai Chi Fan Style) and an initial check in period. In addition to the slow, rotational, fluid movements (1.5 minutes per motion), the women participating in the study were taught to control their breathing. Over the eight weeks, they also underwent blood and had physical fitness evaluations.
The findings? Tai Chi training improved balance, flexibility and leg extension strength in all of the women regardless of menopausal status. LDL cholesterol was also lowered. And, as mentioned, markers for antioxidant activity increased significantly while a marker for heart disease risk decreased.
Tai Chi is low impact and is especially valuable for women who may not be physically able to boost their aerobic routines. What’s more, once mastered, it can be practiced in the privacy of one’s own home. Once again, the mind-body connection proves to be pretty darn cool and important to health and wellness! This time, it might take some practice but perseverance rules the day! “There is no mystique to Tai Chi Chuan. What is difficult is the perseverance. It took me ten years to discover my chi, but thirty years to learn how to use it. Once you see the benefit, you won’t want to stop.” – Ma Yueh Liang
Read MoreAchy breaky joints
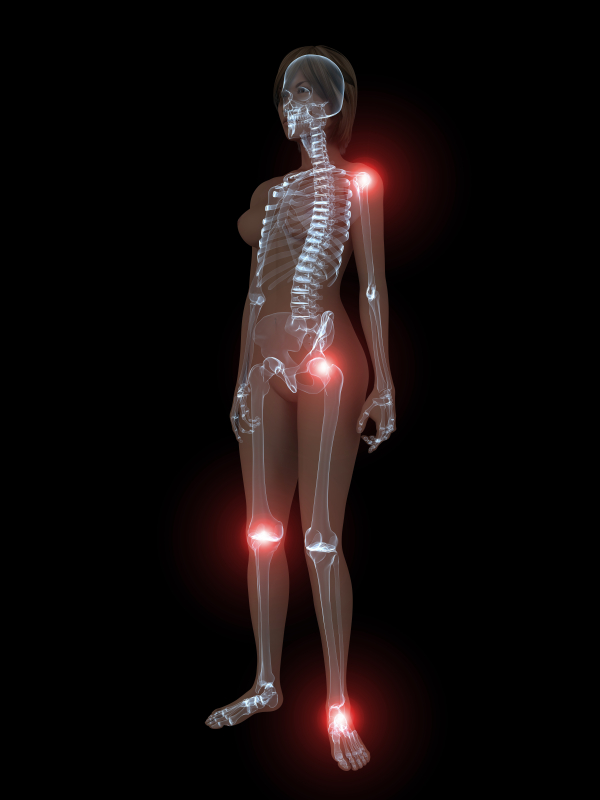 Are you consistently achy? Have you been told that you have fibromyalgia? According to research published in Maturitas, not only are middle-aged women prone to achy muscles and joints that might be otherwise known as fibromyalgia, but, those aches and pains may actually be related to hormonal changes. Indeed, when they reanalyzed information collected from over 8,300 women between the ages of 40 and 59, they learned that muscle and joint aches during this time period were significantly related to menopausal symptoms — not only did more than half of the women (63%) suffer from muscle and joint achiness, but, it appeared to double in prevalance in women ages 55 to 59 compared to their younger (40 to 44 year old) peers. Moreover, it tripled in women who were five years into menopause compared to the same group of women.
Are you consistently achy? Have you been told that you have fibromyalgia? According to research published in Maturitas, not only are middle-aged women prone to achy muscles and joints that might be otherwise known as fibromyalgia, but, those aches and pains may actually be related to hormonal changes. Indeed, when they reanalyzed information collected from over 8,300 women between the ages of 40 and 59, they learned that muscle and joint aches during this time period were significantly related to menopausal symptoms — not only did more than half of the women (63%) suffer from muscle and joint achiness, but, it appeared to double in prevalance in women ages 55 to 59 compared to their younger (40 to 44 year old) peers. Moreover, it tripled in women who were five years into menopause compared to the same group of women.
About 16% of these women said that their symptoms were severe or very severe. And importantly, these women tended to display so-called epidemiological characteristics, things like lower socioeconomic status (and by default, less likely to have the means to pay for better healthcare) or a history of psychiatric care. Regardless, there also appeared to be a direct correlation between feeling less healthy and having severe muscle and joint aches. And, women who had surgical menopause carried an even higher risk of presenting with worse joint symptoms.
Study findings also showed that the more intense menopause symptoms were, the more severe muscle and joint aches appeared to be; up to 60% of women with severe vasomotor symptoms also reported severe to very severe aches and pains.
It is possible that the central nervous system has some sort of role, as it impacts both symptoms and joint and muscle pains. Another commonality is that among women with fibromyalgia, symptoms like weakness, anxiety and insomnia — also seen during menopause — are present.
So where are the holes? Because of the study design, there is no cause and effect conclusion at play; in other words, researchers can’t unequivocally say that menopause causes aches and pains. Moreover, the tools used to evaluate muscle and joint pain are actually the same as those relied on to evaluate menopausal symptoms, which means that accuracy may come into question. Still, what they did learn is that hormone therapy reversed or lessened pain severity, meaning that menopause does appear to play some sort of role.
Meanwhile, if you are feeling especially achy and you are in the throes of menopause, it is very possible it’s not in your head. Talk to your practitioner, And consider mind-body strategies such as meditation, QiGong and yoga, which have been correlated with reductions in pain.
Read More