Wednesday Bubble: Sexual health and hypnosis
You’re getting verrrrrrry…
turned on?
According to a newly reported study during this month’s American Psychological Association Annual Meeting, hypnosis might be the very thing to improve sexual desire and satisfaction.
If you step back, it does make sense. As I’ve written previously, hypnosis may help alleviate the frequency and severity of hot flashes. Think about it: fewer flashes may lead to better sleep and less stress. Both may beget a greater interest in being close, since hot flashes have been alleviated. According to the lead researcher, Dr. Gary Belkin, the warmth from closeness can trigger a hot flash, although admittedly, this is the first I’ve heard of it.
Still, the study, which examined the effect of hypnosis, appeared to suggest significant improvements in overall sexual health. 187 postmenopausal women participated in five weekly hypnosis relaxation sessions in which they received direct and indirect suggestions for relaxation, coolness and mental imagery or structured attention sessions that entailed supportive counseling. They also rated sexual desire and pleasure, symptoms and the degree to which hot flashes appeared to interfere with sex both at the beginning and end of the study.
Elkins reports that after 12 weeks, hypnotic relaxation therapy appeared to significantly improve sexual satisfaction and pleasure and decrease discomfort. And while he acknowledges that postmenopausal sexual health can be affected by factors other than hot flashes, e.g. fatigue, self esteem, partner’s health and the quality of the relationship, the positive effects of hypnosis warrants more research.
Meanwhile, perhaps self-hypnosis can help get those juices flowing again? Who knows?
Read More
The present of being present: cortisol and mindfulness meditation
 It seems that I write about stress a lot on Flashfree. Perhaps that is because like many, my life — namely my work — can be very stressful from time to time. However, according to the American Psychological Association, I’m not alone; most Americans suffer from moderate to high stress and the problem does not appear to be going away. Moreover? Work issues are the primary stressors in 77% of people.
It seems that I write about stress a lot on Flashfree. Perhaps that is because like many, my life — namely my work — can be very stressful from time to time. However, according to the American Psychological Association, I’m not alone; most Americans suffer from moderate to high stress and the problem does not appear to be going away. Moreover? Work issues are the primary stressors in 77% of people.
From a midlife perspective, stress and its related hormone, cortisol, can cause a lot of health-related problems. In fact, not only does cortisol promote a fat dump in the midsection, but experts say that overexposure to cortisol and other stress hormones has a cumulative affect, leading to heart disease, sleep issues, digestive issues, obesity, depression and worsening of skin conditions. It’s critical to counter stress’ negative effects before they take their toll and start to do permanent damage. One important strategy to achieve a better balance is meditation.
Fortunately, a team of researchers at UC Davis’ Center for Mind and Brain are devoting time to studying psychological and physiological processes in order to explain the benefits of meditation. The framework for this effort is the Shamatha Project, which is apparently the most comprehensive meditation study ever undertaken. Most importantly, this scientific twist on a centuries old practice may ultimately elevate meditation’s place in Western medicine.
To better understand the effects of meditation on stress, the research team recently took 60 people (between the ages of 22 and 69) who had some prior experience with meditation, measured cortisol and body mass index and their current degree of ‘mindfulness,*’ and then randomly assigned them to a three month meditation retreat or a waiting list. Those on the waiting list participated in the same, three-month retreat at a later date. (*Participants completed a mindfulness questionnaire that measured the degree that these people directed their cognitive resources to sensory experiences and how often they drifted, as well as their ability to let go of distressing thoughts.)
At the retreat, the group met two times a day for one hour, guided sessions and the rest of the time (around 6 hours) practiced solo meditation in 20 to 30 minute increments. Meditation practices were focused on mindful breathing and relaxation and promoted compassion and kindness toward others. Overall, the emphasis was on present awareness rather than meandering into the future of ‘what if’s.’ During the middle of the retreat, all were encouraged to enter into silence for a period of about four weeks. Aside from scheduled meals and group meditations, everyone was on their own to decide sole meditation, exercise and free time.
Did learning how to direct and focus attention away from uncontrolled, ruminating thoughts and worry and toward a chosen target reduce cortisol levels? The researchers say that they found a correlation between a high score for mindfulness and a low score in cortisol, both before and after the retreat. The results were greatest for participants who were able to achieve the greatest increases in mindfulness, that is, the more that they reported directing their thoughts to the present/immediate experience, the lower their resting cortisol levels were. Participants also experienced large improvements in overall wellbeing, daily mood and emotional functioning.
While the findings do not prove cause and effect, they do suggest that changing the mind paradigm to focus on the now rather than the future may ultimately help to reduce our tendency to think about the past or worry about the future and in turn, counter excessive cortisol release.
Tonya Jacobs, a postdoctoral researcher and the study’s lead author, explains that “the idea that we can train our minds in a way that fosters healthy mental habits and that these habits may be reflected in mind-body relations is not news; it’s been around for centuries. But, accumulating evidence might help the idea — that the present is the best present we can give ourselves — be better integrated into Western mentalities and health practices.
Mindful meditation may ultimately prove to be one of our strongest defenses against stress and its companion, cortisol!
Read MoreMonday Musings: The More Things Change
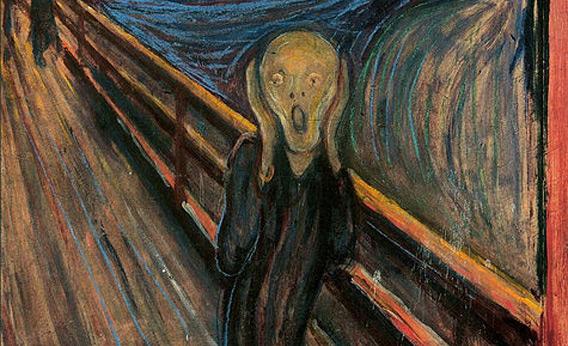
The Scream. Edvard Munch 1895.
The ‘Change.’ A time for ‘hysteria.’
I kid you not.
All joking aside, if you trace the history of the menopause, it has long been associated with loss, decline and decay, something is abhorred and shunned in society. And as I wrote earlier this year, in “response, marketers and the media have perpetuated and pathologized what author Louise Foxcroft (in her book, ‘Hot Flushes, Cold Science’) refers to as “one more feature in a woman’s linear life history, an inevitable and natural phenomenon, one more thing to negotiate and nowhere near as astonishing or potentially problematic as pregnancy.”
Even the British Medical Journal has been in the game, publishing a piece in 1937 that highlights how profound an impact the ‘Change’ can have a woman’s ability to function:
“Practically every menopausal woman becomes aware of certain mental clumsiness, an inability to cope with the ordinary problems of daily life, and a tendency to “give in.” The realization of her shortcomings is worrying, and she readily becomes depressed. Emotional instability is well defined, and the patient reacts to trivial situations with rather surprising attacks of laughter or tears. She is subject to rapid and frequent changes of mood: at one moment she will be unbearably irritable, at the next, pathetically contrite. There may be marked changes in personality and severe attacks of mental depression, sometimes lasting for days, during which the patient may become suicidal. A condition of hypochondriasis, which is particularly distressing to those around her, may develop out of the complicated syndrome, even in the milder cases, and persist for the remainder of the patient’s life.”
No wonder pharmaceutical manufacturers started pushing thorazine and benzadrine.
If wandering around in a drugged out state doesn’t calm you down or pep you up, the general 1937 approach might. In fact, I am of the mindset that modern medicine may need to take a page from 1927 clinician Dr. PMF Bishop:
“Assistance can be rendered by the members of the patient’s household. Her husband and relatives should be told that she is passing through a difficult phase of life and that they should therefore be tolerant and sympathetic in their dealings with her. She should be shielded as much as possible from domestic worries, and sometimes a holiday away from her household duties is beneficial, thought i may be harmful if she is a woman of forceful personality who will worry over the conduct of her home in her absence. She should be encouraged to pursue any hobby which will prevent her from becoming introspective about her condition. She may suffer from a secret fear that her symptoms are due to cancer, and it is wise for her doctor to reassure her specifically on this point.”
So, what is the point of my Monday musing? Menopause is still viewed as an hysterical condition in many circles. The trouble is, the recommended solution is HRT (mind you, even Dr. Bishop writes about estrogen replacement) and rarely do practitioners recommend that the woman simply take a long holiday away from the stressors of her mind and body. Relaxation can help; I’ve shown you the data on Flashfree time and again.
Just think if someone could put THAT in a bottle.
Read More
Just breathe
Want to reduce the frequency of your flashes?
Just breathe.
I’m serious. Just as serious as Mayo Clinic researchers who recently published a study about paced breathing in the online version of Menopause. If you are unfamiliar with the term, paced breathing refers to slow, deep breathing from the diaphragm.
Although experts are still unclear as to the underlying cause of hot flashes, they believe that they are related to a dysfunction in a process called ‘thermoregulation;’ this is the ability to keep our body temperature in a steady state, even when the environment changes. A decrease in estrogen levels, coupled with increased activation of the sympathetic nervous system (which assists in controlling the body’s functions and the fight or flight mechanism) narrows the natural comfort zone and tolerance for temperature fluctuations. Voila! A flash is believed to be born.
So where does paced breathing fit in? Here’s the interesting part: paced breathing decreases the activity of the sympathetic nervous system. So, when the nervous system goes into overdrive, paced breathing can theoretically calm the waters. However, as we go through our busy lives, is regular paced breathing even feasible?
To find out, 105 women were provided with either audio recordings of chimes that paced their breathing or were asked to simply breathe normally. All of the women reported having at least 14 or more hot flashes a week, and they also a history of breast cancer. Women assigned to paced breathing were asked to use their audio recordings either once or twice a day and practice taking 6 breaths per minute for 15 minutes. The other women practiced regular breathing (14 breaths per minute) for 10 minutes a day. All of the women kept a daily hot flash diary.
Over nine weeks, women who practiced paced breathing twice a day reported reductions in daily hot flashes by 52%. Paced breathing practiced once a day reduced hot flashes by 42%. What’s more, women who didn’t slow their breathing deliberately but simply focused on it 10 minutes a day reduced the frequency of their hot flashes by 46%; this suggest that focusing can help alleviate symptoms and that some sort of placebo effect is at play. Still, other studies have similarly reported reductions in hot flash frequency by as much as 50% using progressive muscle relaxation which also has a positive effect on the nervous system. In fact, I just wrote about relaxation and flashes last week.
Most of the women found it challenging to fit 30 minutes of paced breathing into their day, which suggests that perhaps intensifying the effort once a day can provide the same beneficial results. For the most part, there was some initial dizziness but it was mostly mild and likely the result of significantly slowing breathing; more practice would probably help to ameliorate this effect.
It seems to me that it is possible to move away from drugs and towards the body and mind to balance our internal thermostats. The bottom line appears to be that a bit of effort can potentially a long way towards solving a problem that has long eluded the medical community.
Just breathe.
Read MoreWednesday Bubble: Relax, just do it.
You think that hormones are the only solution to hot flashes?
Think again!
This is not the first time that I have reported that the mind-body connection is an important key to menopausal symptoms. Moreover, it probably won’t be the last. In fact, in a second study published within the past 18 months in Menopause journal, researchers are again moving away from hormones and moving towards applied relaxation. (A related study topic-wise can be found here.)
This time, Swedish researchers assigned 60 women in menopause to either ten sessions of group therapy combined with relaxation or to no intervention for three months. All of the women had been experiencing moderate to severe hot flashes at least 50 times a week. During the 10 group therapy relaxation sessions, the women were taught to methodically move through the body’s muscle groups and use breathing techniques to systematically relax each group. They were then provided with exercises to practice daily at home, with the the goal being to learn the relaxation method and self-manage their symptoms. During this period, all participants kept a regular hot flash diary and filled out a quality of life survey on three different occasions. They also provided the researchers with a sample of their saliva.
The findings? Women practicing daily relaxation and engaging in regular coaching sessions actually reduced their daily hot flash count from an average of 9.1 to 4.4 a day; that’s about a 50% reduction. In the group of women who had no interventions, a reduction in daily hot flashes was also observed but on average, these women experienced less than two fewer flashes a day; this is likely the result of what researchers consider a ‘placebo effect.’
More importantly, benefits of relaxation remained for at least three months after the study ended and the final therapy sessions. The women who practiced relaxation also reported improvements in overall wellbeing and quality of life, including sleep and memory. What’s more, saliva testing showed reductions in cortisol; as I’ve written previously, stress leads to cortisol release and ups the hot flashes ratio. Once that cycle starts, who knows how long the endless loop plays out?!
Time to stop the loop? Forget the drugs. Breathe deeply, exhale and repeat. Just do it.
Read More