Wednesday Bubble: Sham?

Today’s Bubble troubles me because it’s a bit personal. You see; I want to believe.
Reporting in the Climacteric journal of the International Menopause Society, researchers say that a thorough review of scientific studies examining acupuncture and hot flashes failed to reveal any specific effects. So, is acupuncture no more effective than sham acupuncture, i.e. placebo?
In this report, which appeared in the February 2009 edition of the journal, researchers searched studies published in 17 databases in different languages. Of the six well-designed trials that were ultimately included in their review, four compared regular acupuncture with sham acupuncture, in which a practitioner will insert needles on acupuncture points that are not relevant for treating hot flashes. The results: none of these trials showed any benefit of acupuncture in terms of frequency or severity of hot flashes.
Only one trial showed any favorable effects: this particular study tested acupuncture against needles that were place on non-relevant points but not inserted into the skin.
So, what can we conclude from these findings?
The researchers say that controlled studies, in which the environment is scientifically designed to mimic real life, fail to show any specific effects of acupuncture for controlling hot flashes. However, they do not appear to believe that this is the end all to be all. Instead, they call for more rigorous trials to further investigate the use of acupuncture for hot flashes.
Perhaps the ACUFLASH trial will shed more light.
What are your experiences with acupuncture? Have you used it specifically to treat hot flashes?
Read MoreWhat’s cooking?!

In college, we had an oven that was malfunctioning. Consequently, one of my roommates was able to fry an egg on its surface without the use of any burners.
Who knew that 30 years later, there would be an alternative?!
Happy Friday!
Read MoreSt John’s Wort, Quality of Life & Hot Flashes

Can St. John’s Wort improve quality of life during perimenopause?
While the benefit of St. John’s wort for treatment depression and other mood disorders remains inconclusive, there is new evidence that it might be useful for symptoms of perimenopause that affect quality of life, namely hot flashes.
In a small study published in the February 3 Advanced Edition of Menopause, researchers randomly assigned 47 perimenopausal women experiencing 3 to 5 hot flashes daily to 900 mg St. John’s Wort extract three times daily or placebo. All study participants were asked to keep daily diaries noting the frequency and intensity of their hot flashes. Quality of life and hot flashes scores were also calculated.
At three months, women who had been taking St. John’s Wort reported significant improvements in menopause-specific quality of life and significantly fewer sleep problems. They also experienced improvements in daily hot flash frequency and hot flash scores.
Although the researchers caution that this is small study and that larger trials are needed,they say that St. John’s Wort may improve quality of life in ways that are important to perimenopausal women.
About St. John’s Wort
In addition to controversy over its effectiveness in treating depression, experts recommend against taking St. John’s Wort at the same time as alcohol, narcotics, amphetamines, tyrosine supplements, flu medicines and foods containing tyramine (e.g. yeast, aged cheese, eggplant, soy sauce). St. John’s Wort can also interact with prescription antidepressants, oral contraceptives and certain medications that thin the blood. More information about St. John’s Wort, its side effects and risks can be found here.
As with any herbal preparation, it’s critical to speak to a healthcare practitioner before embarking on therapy. Acupuncturist and Chinese Medicine Specialist Elaine Stern has a few tips with regards to what you should look for.
In the interim, keep an eye out for more news about St. John’s Wort. These results are encouraging news for hot flashers!
Read MoreShe’s got moxi
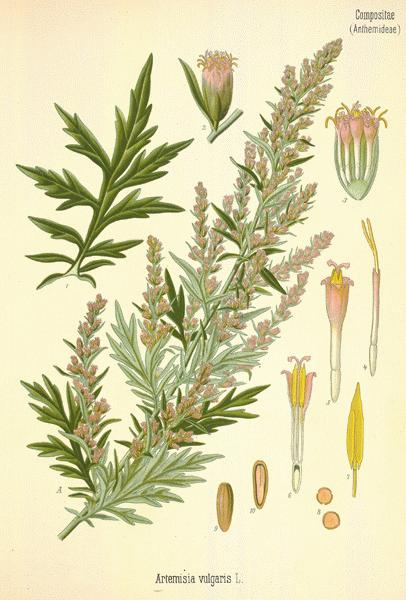
Have you heard of or experienced moxibustion? Moxibustion is a technique used during acupuncture in which mugwort (or artemsia vulgaris) is burned to warm certain regions or acupuncture points. It can be direct (in which the moxa is placed directly on the acupuncture point) and indirect (in which the moxa is palced approximately 1 to 2 cm above the acupuncture point). The purpose of moxibustion is to encourage better blood and energy flow through the area to promote healing.
A study in the March 13 advanced online edition of Menopause suggests that moxibustion plus acupuncture can reduce both the frequency and severity of hot flashes.
In this study, researchers randomly assigned 51 women, ages 45 to 60 years who experienced at least 5 moderate to severe hot flashes daily to:
- 14 sessions of indirect moxibustion plus acupuncture at points consistent with evidence from clinical practice experience
- 14 sessions of indirect moxibustion plus acupuncture at points consistent with evidence from published literature
- no treatment
To ensure that researchers were able to distinguish between general improvements and improvements resulting from treatment, all study participants had to go through a 1-week period during which time they used not treatments at all.
Study findings showed that compared with no treatment at all, women in both moxibustion groups experienced significantly reductions in hot flash frequency (roughly 60% in both groups), and continuous reductions in hot flash severity through the fourth week of the study (by as much as 50%). 10 participants experienced side effects due to the moxi smoke (e.g. fatigue, stomach upset, flare-up and headaches ) and 5 reported burns to their skin).
Notably, women receiving moxibustion along points directed by published literature also experienced more improvements in quality of life scores, particularly as they related to symptoms and psychosocial issues.
This study appears to indicatethat moxibustion may help to enhance acupuncture’s effect on hot flashes during the menopause. Clearly, more studies with larger samples are needed.
Read MoreTiming is everything
Headache, irritability and mood swings….they’re going to disappear someday. Promise.
Research findings show that certain symptoms commonly linked with menopause decline linearly, meaning that as you move through the transition, those bothersome symptoms will move with you and then gradually diminish. Phew!
A study that appeared in Obstetrics & Gynecology early last year showed a direct association between menopausal symptoms and reproductive hormones at any given time during the menopause. Researchers evaluated menstrual bleeding patterns, symptoms and levels of estradiol, follicle-stimulating hormone (FSH) and testosterone in women over a nine-year period. Stages of menopause were analyzed based on bleeding patterns. All women underwent structured interviews, completed symptoms questionnaires and were followed for bleeding dates and hormone measures.
The results showed that headache was significantly associated with stage of menopause, declining in the pre- to postmenopause transition. Mood swings and irritability were both associated with declining FSH levels. Additional analyses also revealed a link between PMS, perceived stress and all three of these symptoms (i.e. headache, irritability and mood swings).
So what about other symptoms like hot flashes and night sweats and depression? A small percentage of women may have to deal with them a bit longer. In fact, data suggest that they may persist well into the postmenopausal period although the reasons are not entirely clear.
Read MoreWhat’s your sleep number?

[Rembrandt van Rijn, Sleeping Woman, 1658]
On a scale of 1 to 5 would you say that your sleep number (the quality of your sleep) is:
- nonexistent, I never sleep
- occasional, I sleep one or two nights a week
- obstructed, I sleep but I wake up regularly throughout the night
- pretty good, I rarely wake up
- great, I typically sleep through the night
If you are like most peri- post menopausal women, it’s likely that you rate the quality of your sleep about a “3. ” In fact, a review in the journal Current Neurology and Neuroscience Reports suggests that 28% to 64% of peri- or postmenopausal women have some form of sleep disturbances that may aggravated by sleep apnea, periodic limb movements syndrome (restless leg syndrome) and psychological distress (anxiety, major depression).
One of the primary causes of sleep disruption during menopause is declining estrogen levels, which increase peripheral and central temperature, dilate blood vessels and lead to hot flashes. Unfortunately data also suggest that hot flashes double the time spent awake although ironically, they often follow rather than proceed awake times.
More good news: both sleep apnea and periodic limb movements syndrome increase with age. Menopausal women are espeically at risk due to declining progesteron levels and increased body mass index (and associated increases in neck circumference). Both sleep apnea (in which the airways become partially or totally obstructed) and periodic limb movements obviously interefere with sleep quality. In fact, sleep researchers have documented apnea, restless leg syndrome or both in up to 53% of women between the ages of 44 and 56.
The evidence is less certain for mood disturbances and sleep, although studies have shown clear links between reproductive hormonal changes and clinical depression in women going through menopause. What’s more, women in menopause who are clinically depressed have reported more frequent and longer times awake than those who do not have any mood disturbances.
Steps to take
I’ve written previously on this issue and there are a variety of non-pharmacologic steps that might improve sleep quality including standardized herbs and acupuncture.
Hypnosis, relaxation techniques that include breathing and/or biofeedback) may also assist. These strategies are part of a larger approach called cognitive-behavioral therapy for insomnia (CBT-I) which in a small study, was found to significantly improve anxiety, depression, partner relationships, sexuality and hot flashes in menopausal women.
Notably, the benefit of HRT for sleep/mood disturbances remains unclear and studies are inconclusive.
As with any issue associated with menopause, it’s critical to speak to a health practitioner about the issue so that the course of therapy can be safely individualized and personalized.
What about you? How’s your sleep? And what are you doing about it?
Read More





