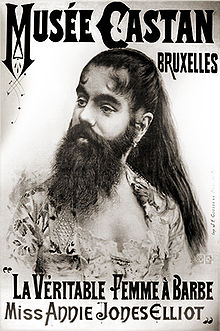
Hairy kiri…sexual desire and hairs on your chinny chin chin
Yes, I am taking poetic license with the Japanese term “Hara-Kiri” which literally means to cut or slice the stomach. This phrase has been hijacked by slangers who refer to it as ‘hari kari,’ to off oneself or commit suicide.
I propose that using testosterone in hopes of improving sexual desire is a great way to cut off one’s wellbeing and sense of self Chi, leaving hairs on the chinny chin chin and other undesirable locations.
Hairy kiri? You bet!
Back in 2008, I wrote about Intrinsa, a testosterone patch that was tested in a study of 841 postmenopausal not currently on hormone replacement therapy to test its effects on sexual desire after about a half a year’s use. The results, which were published in the New England Journal of Medicine, showed that compared to a dummy patch, using low or high dose Intrinsa was associated with significant increases in sexual desire and a decline in sexual distress. Overall, the higher dose patch led to modest improvements in sexual function. In other words, wearing a patch was significantly better than using nothing at all but not life-shattering in terms of improving sexual function. However, the caveat was unwanted hair growth, which occurred in about a third of women using the higher dose patch and in about 23% of women using the lower dose.
Once I delved further into androgens and women, I learned that while it has been suggested that local circulating levels of androgens are associated with low sexual desire and sexual dysfunction, the data are contradictory. Moreover, in a fairly recent scientific review, researchers say that no single androgen predicts which women will have sexual dysfunction, making it even harder to address, right? What’s more, they also note that laboratory studies have only limited value and aren’t routinely recommended.
Looking more closely at different formulations of androgens like testosterone, e.g. patches, oral tablets, implants and injections, experts have found that the major side effects are unwanted hair growth and acne. Both are related to dose and how long treatment lasts, and disappear once treatment is stopped. And while rates of hair growth are definitely lower for patches in general (as few as 7% to as high as 23%), as many as 36% of women who use oral testosterone have unwanted hair growth. Among those receiving implants, pellets or injections the number is also high: 20%.
Let’s face it; the trouble is testosterone is that it may only address a miniscule amount of factors affecting a woman’s libido and in literally leave a trail in its place. Don’t know about you but I think it’s a hairy kiri proposition. A few more notches on the desire scale and a few more hairs in your chin, on your chest and lord knows where else.
Committing hairy kiri ain’t for sissies; that’s for sure!
Read More
Wednesday Bubble: Are you in the moo? Sex and a sense of purpose
What are we bursting this week? How about midlife and sexual desire. Frankly, I’ve got sex on the brain, sex in midlife, that is. And what we need to do to insure that it continues to be enjoyable, that we desire it and that we please our partners as much as we hope that they please us. Consequently, I am reposting this piece from earlier in the year, with the hope that with a sense of purpose, you’ll become more in the moo. Or mood. Whatever the case may be.
Sexual desire. In midlife, sexual function and sexual desire aren’t well understood, primarily because there are so many factors that enter into equation. This may be why certain silver bullets, like a female viagra, has failed to show any significant improvements in the desire department. And yet, researchers continue to accrue more information about the things that influence desire in women, ranging from the quality of intimate relationships to social support and overall wellbeing. The manufacturer who discovers a pill that addresses all of these will have struck gold. Meanwhile, back in reality, as many as 75% of women in midlife rate sexual health as important enough to warrant further exploration.
Fortunately, we may have another piece of the puzzle: ‘sense of purpose,’ which appears to be associated with greater wellbeing, happiness, life satisfaction, self-esteem, personal growth and optimism. A sense of purpose also appears to improve health, prevent certain diseases and may even improve cognitive function, thereby staving off mental diseases associated with aging. In a study that appears in the online version of Menopause, 459 menopausal women who were sexually active with a partner were followed over three years. Each year, they were asked about their emotional wellbeing (including their general mood, anxiety and depression as well as how often they engaged in and enjoyed sexual activity (specifically desire, type of activity and hugging and kissing). In the final year, they took a test that rated their sense of purpose on a five point scale ranging from ‘there is not enough purpose in my life’ to ‘the things I do are all worthwhile.’
The findings?
A greater sense of purpose equaled a great enjoyment of sexual activities, independent and regardless of other specific life circumstances. In other words, psychosocial functioning, e.g. social support, quality intimacy and overall wellbeing influenced the quality of these women’s sexual lives. On the other hand, menopausal status and use of hormone therapy did not appear to play a significant role in how often women engaged in sex or if they enjoyed it. This is important, as it means that psychosocial wellbeing may ultimately be more important than hormones.
In so far as the desire to engage? Women who were younger, had more social support, felt better about themselves and weren’t suffering from vaginal dryness tended to want sex more than their older peers who didn’t enjoy these factors.
Not surprisingly, many of the factors that researchers stress may help desire and engagement are associated with greater nitric oxide levels, which Dr. Christina Northrup says can help combat sexual dysfunction and improve pleasure.
When it comes to sex in midlife? It may help to think ‘sense of purpose,’ a real sense of purpose, now. (Poetic license, Chrissie!) I’m all for it if improves activity and desire without drugs.
Read MoreOn breast cancer screening. Guest post by Dr. Elaine Schattner
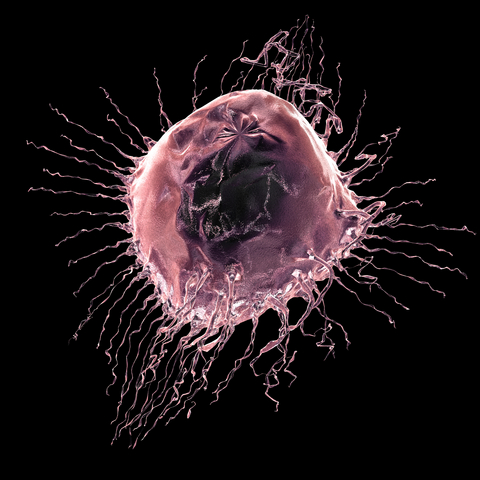
Mammography screening. Should you? Or shouldn’t you?
A few weeks ago, I received a letter in the mail from the clinic where I get my mammography. Rather than the expected ‘all is fine,’ the clinic was requesting that I call to schedule another screening due to abnormal findings. Not only was this not the way that I wanted to receive news that something might be wrong, but, I opened the letter at 4 pm on a Friday afternoon, giving me little time to get over the initial shock and then get on the phone to see if I could learn a bit more before the clinic closed for the weekend.
Mammography screening has been in the news quite a bit over the past year, with lines being drawn between experts who say that screening doesn’t save lives and women who want their mammograms regardless of the facts. I happen to fall on the latter side of the aisle and while I suffered a lot of anxiety before I had a second screening, not knowing would have been even worse. (FYI – it turned out fine.)
Recently, my friend Dr. Elaine Schattner, a trained oncologist, hematologist, educator and journalist, wrote about a new review that I believe that every woman should read before deciding whether or not to have a mammogram. It puts some of the controversy into perspective and also provides a much more balanced viewpoint on the risk-benefit ratio. And rather than reinvent the wheel, I asked Elaine if I could re-run the post on Flashfree. Please share it far and wide; it’s important.
With little fanfare, the NEJM published a feature on breast cancer screening in its Sept 15 issue. The article, like other “vignettes” in the Journal, opens with a clinical scenario. This time, it’s a 42 year old woman who is considering first-time mammography.
The author, Dr. Ellen Warner, an oncologist at the University of Toronto, takes opportunity to review updated evidence and recommendations for screening women at average risk for the disease. She outlines the problem:
Worldwide, breast cancer is now the most common cancer diagnosed in women and is the leading cause of deaths from cancer among women, with approximately 1.3 million new cases and an estimated 458,000 deaths reported in 2008.(1)
On screening:
The decision to screen either a particular population or a specific patient for a disease involves weighing benefits against costs. In the case of breast-cancer screening, the most important benefits are a reduction in the risk of death and the number of life-years gained….
She breaks down the data for mammography by age groups:
For women between the ages of 50 to 69 the evidence is clear, she says. For those over 70, there are little data to support breast cancer screening. There’s a consensus that screening isn’t appropriate for women with serious coexisting illnesses and a life expectancy of less than 5–10 years.
For those between the ages of 40–49, Warner challenges the revised 2009 USPSTF recommendationson several counts. She critiques those authors’ weighting of data from the Age trial of 161,000 women, emphasizing the use of an antiquated (single view) mammography technique and flawed statistics. She considers:
…However, this change in remains highly controversial,22, 23 especially because of the greater number of years of life expectancy gained from preventing death from breast cancer in younger women. According to statistical modeling,19 screening initiated at the age of 40 years rather than 50 years would avert one additional death from breast cancer per 1000 women screened, resulting in 33 life-years gained.”
What I like about Warner’s analysis, besides its extreme attention to details in the data, is that she’s not afraid to, at least implicitly, assign value to a procedure that impacts a young person’s life expectancy relative to that of an older person.
She goes on to consider digital mammography and the Digital Imaging Screening Trial (DMIST [NCT00008346]) results. For women under 50 years, digital mammography was significantly more sensitive than film (78% vs. 51%).
The article is long and detailed; I recommend the full read including some helpful tables, with references to the major studies, and charts.
In concluding, the author, who admits receiving grant support from Amersham Health (a GE subsidiary), consulting fees from Bayer and lecture fees from AstraZeneca, returns to the hypothetical patient, and what might be said to a woman in her 40s who lacks an outstanding risk (such as a genetic disposition or strong family history):
…Mammography screening every 2 years will find two out of every three cancers in women her age, reduce her risk of death from breast cancer by 15%. There’s about a 40% chance that further imaging (such as a sonogram) will be recommended, and a 3% chance for biopsy with a benign finding.…
In my opinion (ES) this is key – that the chances of a false positive leading to biopsy are only 3% for a woman in her 40s. If those biopsies are done in the radiology suite with a core needle, every 2 years for women of average risk, the costs of false positives can be minimized.
About the author…Dr. Elaine Schattner is a trained oncologist, hematologist, educator and journalist who writes about medicine. Her views on health care are informed by her experiences as a patient with scoliosis since childhood and other conditions including breast cancer. Elaine is a Clinical Associate Professor of Medicine at Weill Cornell Medical College in New York City where she teaches part-time. Her blog, Medical Lessons, is geared towards dissecting and providing commentary on how healthcare news is comunicated in order to foster learning and help bridge the gap between patients and doctors.