Wednesday Bubble: Timeout
Back in 2009 I posted a story about a woman’s death being blamed on menopause. It seems especially poignant a day after World Menopause Day, a day unlike any others, when we put down our prejudices and celebrate everything menopause.
As my grandmother would say “oy vey.”
How about we focus on how, as women, we are constantly manipulated by ‘disinterested’ parties? How about we call “timeout?”
A bit of context…
In 2009, the BBC ran a story about a woman who committed suicide. The headline read:
“Woman’s Death Blamed on Menopause.”
“A woman who refused to take hormone replacement therapy died while suffering a menopausal episode, an inquest had heard. Margaret Drew…was killed when she walked out of her family home on to a nearby railway line and was hit by a train…There is no trigger to this at all, except hormones making her do things that she normally wouldn’t do, Dr. Carlyon [Cornwall Coroner) concluded…”
Menopause. The silent killer. Oh really? Drew’s husband claims that his wife was “delightful, lovely and friendly” 99% of the time; the other 1% she’d become “totally irrational.” Yet, she refused to try HRT, he says. On the day of her suicide, he said that his wife was “clearly angry about something.”
Something.
Obviously, the conclusion is that that the “something” is hormones. This reminds me of vintage advertising copy that conveys the simple message that a pill a day can cure all that ails, wipe away the tears, mood swings and instability so that women can “transition without tears” (or better yet, without killing themselves).
Notably, a search in the National Library of Medicine’s PubMed database turned up only one recent study specifically dealing with suicide ideation across reproductive stages. In it, researchers compared data in 8,794 women, and found an increased risk of thinking about suicide among women during perimenopause, not before or after entering menopause. These findings remained after controlling for risk factors such as anxiety and mood disorders. HOWEVER, the researchers noted that the study design did not allow them to form any definitive conclusions about the specific reasons for thinking about suicide.
Another search yielded information that the risk for a major depression increases during perimenopause, primarily as the direct result of vasomotor symptoms. The same does not hold true for women before menopause begins or once they enter menopause. Note that while major depression is a risk factor for suicide, not everyone who is depressed will actually kill themselves.
Are hormonal fluctuations the sole cause of such deep unhappiness that women want to kill themselves? Or their careers?
Let’s look at a more recent story that appeared this week in the Denver Post.
“Former Elbert County assessor blames menopause medications for crimes, is sentenced to 60 days in jail, fined $10,000”
“Elbert County Judge Jeffrey Holmes might have thrown the book at former county assessor P.J. Trostel just for her management skills alone. Instead, he sentenced Trostel today to 60 days in county jail, three years of probation and 200 hours of community service on two felony counts…In asking for leniency, Trostel and her lawyer said a variety of factors led her to make bad decisions. Those included depression, symptoms from menopause, medications and stress from family and work. “Some of the things I don’t even have an answer,” Trostel said. “I know I made terrible judgments and decisions.”
It sounds as though Trostel would have done better with different legal representation. And a sounder argument.
And while Trostel is chewing on that concept for the next six years while incarcerated, perhaps we can start to change the paradigm and focus on the ills of the Menopause Industrial Complex, disinterested parties who perpetuate societal myths that menopause is a disease that requires treatment and that as women, our attitudes, belief systems and actions are hormonally-based and driven. That we are hysterical beings who need guidance on how to find our way and fulfill our dreams, realize our paths, but only if we calm down. That we can’t hold a job down, keep a marriage intact or play nicely with others. That we need a timeout (this would entail a long, long time, by the way).
Seriously though, a timeout from the hype would be a welcome addition to the change, don’t you think?
Read More
Needles and symptoms and a pathway, revealed…more on acupuncture
Click on acupuncture in the tag cloud and you’ll know that I’ve spent a number of years examining and sharing information about important studies on this blog. In some, acupuncture has been shown to alleviate vasomotor symptoms like hot flashes and night sweats, and in others, acupuncture appears to be no better than placebo or sham needles that are placed on accurate points but not actually inserted into the skin. However, I’ve also long argued that by slightly changing the way that we conduct scientific studies in the West and allowing for individualization, observed benefits might be different. Indeed, that’s exactly what researchers have seen with ACUFLASH and you can read more about that trial here.
Less clear that whether or not acupuncture can help symptoms (for the record, I am biased and I believe that over time it can), is HOW it works. The centuries old Chinese medicine paradigm is never so apparent than with acupuncture and although I am not sure why we need to know the ‘how,’ I am fairly certain that until it is revealed, there will be a lot of researchers and health practitioners questioning its validity or utility.
So, this brings me to a wonderful pilot study in the online version of Menopause, exploring that very question: how does acupuncture work on vasomotor symptoms?
In this small trial, 33 perimenopausal and postmenopausal received traditional acupuncture, sham acupuncture or nothing over a period of 12 weeks. The active groups received three treatments per week and all the women reported having at least 7 hot flashes a day. But there’s the rub: the researchers also looked at how traditional acupuncture affected the hypothalamic-pituitary axis (HPA), the part of the body that comprises the hypothalamus and pituitary and adrenal glands, controls digestion, our immune system, mood and emotions, sexuality, and how energy is used and stored. Moreover, this part of the body reacts quite negatively to stress by releasing a hormone known as cortisol. Not surprisingly, women who have very severe vasomotor symptoms tend to produce high levels of cortisol.
What did they learn?
- Most of the benefits, (e.g. reductions in hot flashes) occurred by week five and; hot flash severity and frequency declined by 86% and 78%, respectively in both the real acupuncture and sham acupuncture groups. But while the sham acupuncture group didn’t continue to improve, the real acupuncture group did.
- Likewise, anxiety and depression improved in both of these groups, as did sleep scores.
And the “how?”
It appears, at least from this small study, that acupuncture positively affected levels of cortisol and DHEA, the major steroid secreted by the adrenal glands that affects none other than the body’s production of estrogen. Consequently, if acupuncture helps to control the HPA, and HPA affects vasomotor symptoms, then perhaps scientists have the first clue as to why acupuncture may help certain menopausal symptoms. It also opens up an entirely new avenue for novel strategies to control them.
The bottom line is that there is hope and a new direction that researchers will ideally follow. Ultimately, acupuncture may prove to be even more effective than pharmaceutical strategies for menopausal symptoms and definitely, much safer.
The jury’s still out but it seems a helluva closer to a verdict.
Read More
Wednesday Bubble: Warn me
This week’s Bubble is straight out of the buyer beware files. Introducing Warmi ‘Better Menopause Relief.’
Warmi, according to the manufacturer website, is “a unique vegetable and fruit extract supplement. It contains 85% organic ingredients in a vegetable capsule and is 100% Vegetarian.” Moreover, Warmi provides safe, natural, full spectrum menopause relief” meaning that in a single study of 122 women, Warmi “also enhanced hormonal balance, mood, cardiovascular and bone health, vaginal dryness and intercourse discomfort — even overall quality of life. Many benefits were noted in just 30 days.”
Evidently, Warmi delivers, all that and more.
How, you ask?
Warmi’s active ingredients are:
- Gluocosinates, plant chemicals that are found in cruciferous vegetables such as cabbage, which are believed to help fight cancer and possibly, promote heart health.
- Beta-sitosterol, a substance found in plants and suggested to have properties similar to cholesterol. It is used in some European countries for benign prostatic hyperplasia (enlarged prostate) and according to the Warmi website, has been shown in laboratory animals to have some sort of weak estrogen effect that “may benefit the reproductive system.”
- Hesperidin, a flavonoid found in citrus fruits which has shown promise in laboratory animals to potentially reduce blood pressure and cholesterol and work as an anti inflammatory and produce pain killing effects. The Warmi website says that it may also ‘help bone metabolism.’ Note that this claim is based on one study done in mice, which demonstrated a decline in the loss of bone density.
So, Warmi is made up of cancer and heart protective ingredients, may alleviate pain, and…helps with menopausal symptoms? But how does it work? In the FAQ section of the product website, it says that while “The exact mechanism of Warmi is not fully understood but is believed to be associated with certain estrogen receptors.”
I’m sorry…WHAT?!
All I can think of when I think ‘Warmi’ is “warn me.” Yes, warn me that medical and scientific claims without substantiation are to be questioned, that comparisons to existing alternative strategies are difficult without well-designed research, and that unpublished, unreviewed product data are just that: unpublished, unreviewed and non-vetted.
Forewarned is forearmed.
Enough said.
Read More
Wednesday Bubble: Are you in the moo? Sex and a sense of purpose
What are we bursting this week? How about midlife and sexual desire. Frankly, I’ve got sex on the brain, sex in midlife, that is. And what we need to do to insure that it continues to be enjoyable, that we desire it and that we please our partners as much as we hope that they please us. Consequently, I am reposting this piece from earlier in the year, with the hope that with a sense of purpose, you’ll become more in the moo. Or mood. Whatever the case may be.
Sexual desire. In midlife, sexual function and sexual desire aren’t well understood, primarily because there are so many factors that enter into equation. This may be why certain silver bullets, like a female viagra, has failed to show any significant improvements in the desire department. And yet, researchers continue to accrue more information about the things that influence desire in women, ranging from the quality of intimate relationships to social support and overall wellbeing. The manufacturer who discovers a pill that addresses all of these will have struck gold. Meanwhile, back in reality, as many as 75% of women in midlife rate sexual health as important enough to warrant further exploration.
Fortunately, we may have another piece of the puzzle: ‘sense of purpose,’ which appears to be associated with greater wellbeing, happiness, life satisfaction, self-esteem, personal growth and optimism. A sense of purpose also appears to improve health, prevent certain diseases and may even improve cognitive function, thereby staving off mental diseases associated with aging. In a study that appears in the online version of Menopause, 459 menopausal women who were sexually active with a partner were followed over three years. Each year, they were asked about their emotional wellbeing (including their general mood, anxiety and depression as well as how often they engaged in and enjoyed sexual activity (specifically desire, type of activity and hugging and kissing). In the final year, they took a test that rated their sense of purpose on a five point scale ranging from ‘there is not enough purpose in my life’ to ‘the things I do are all worthwhile.’
The findings?
A greater sense of purpose equaled a great enjoyment of sexual activities, independent and regardless of other specific life circumstances. In other words, psychosocial functioning, e.g. social support, quality intimacy and overall wellbeing influenced the quality of these women’s sexual lives. On the other hand, menopausal status and use of hormone therapy did not appear to play a significant role in how often women engaged in sex or if they enjoyed it. This is important, as it means that psychosocial wellbeing may ultimately be more important than hormones.
In so far as the desire to engage? Women who were younger, had more social support, felt better about themselves and weren’t suffering from vaginal dryness tended to want sex more than their older peers who didn’t enjoy these factors.
Not surprisingly, many of the factors that researchers stress may help desire and engagement are associated with greater nitric oxide levels, which Dr. Christina Northrup says can help combat sexual dysfunction and improve pleasure.
When it comes to sex in midlife? It may help to think ‘sense of purpose,’ a real sense of purpose, now. (Poetic license, Chrissie!) I’m all for it if improves activity and desire without drugs.
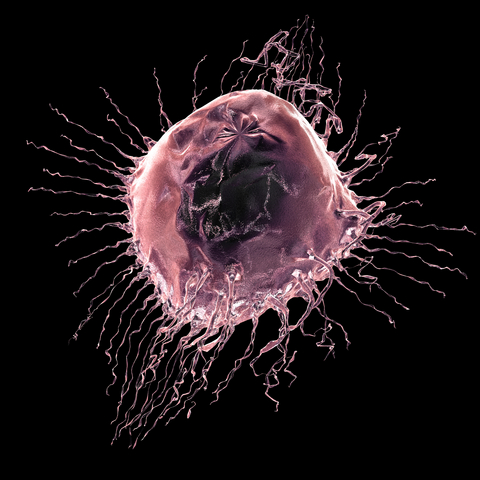
Read MoreOn breast cancer screening. Guest post by Dr. Elaine Schattner
Mammography screening. Should you? Or shouldn’t you?
A few weeks ago, I received a letter in the mail from the clinic where I get my mammography. Rather than the expected ‘all is fine,’ the clinic was requesting that I call to schedule another screening due to abnormal findings. Not only was this not the way that I wanted to receive news that something might be wrong, but, I opened the letter at 4 pm on a Friday afternoon, giving me little time to get over the initial shock and then get on the phone to see if I could learn a bit more before the clinic closed for the weekend.
Mammography screening has been in the news quite a bit over the past year, with lines being drawn between experts who say that screening doesn’t save lives and women who want their mammograms regardless of the facts. I happen to fall on the latter side of the aisle and while I suffered a lot of anxiety before I had a second screening, not knowing would have been even worse. (FYI – it turned out fine.)
Recently, my friend Dr. Elaine Schattner, a trained oncologist, hematologist, educator and journalist, wrote about a new review that I believe that every woman should read before deciding whether or not to have a mammogram. It puts some of the controversy into perspective and also provides a much more balanced viewpoint on the risk-benefit ratio. And rather than reinvent the wheel, I asked Elaine if I could re-run the post on Flashfree. Please share it far and wide; it’s important.
With little fanfare, the NEJM published a feature on breast cancer screening in its Sept 15 issue. The article, like other “vignettes” in the Journal, opens with a clinical scenario. This time, it’s a 42 year old woman who is considering first-time mammography.
The author, Dr. Ellen Warner, an oncologist at the University of Toronto, takes opportunity to review updated evidence and recommendations for screening women at average risk for the disease. She outlines the problem:
Worldwide, breast cancer is now the most common cancer diagnosed in women and is the leading cause of deaths from cancer among women, with approximately 1.3 million new cases and an estimated 458,000 deaths reported in 2008.(1)
On screening:
The decision to screen either a particular population or a specific patient for a disease involves weighing benefits against costs. In the case of breast-cancer screening, the most important benefits are a reduction in the risk of death and the number of life-years gained….
She breaks down the data for mammography by age groups:
For women between the ages of 50 to 69 the evidence is clear, she says. For those over 70, there are little data to support breast cancer screening. There’s a consensus that screening isn’t appropriate for women with serious coexisting illnesses and a life expectancy of less than 5–10 years.
For those between the ages of 40–49, Warner challenges the revised 2009 USPSTF recommendationson several counts. She critiques those authors’ weighting of data from the Age trial of 161,000 women, emphasizing the use of an antiquated (single view) mammography technique and flawed statistics. She considers:
…However, this change in remains highly controversial,22, 23 especially because of the greater number of years of life expectancy gained from preventing death from breast cancer in younger women. According to statistical modeling,19 screening initiated at the age of 40 years rather than 50 years would avert one additional death from breast cancer per 1000 women screened, resulting in 33 life-years gained.”
What I like about Warner’s analysis, besides its extreme attention to details in the data, is that she’s not afraid to, at least implicitly, assign value to a procedure that impacts a young person’s life expectancy relative to that of an older person.
She goes on to consider digital mammography and the Digital Imaging Screening Trial (DMIST [NCT00008346]) results. For women under 50 years, digital mammography was significantly more sensitive than film (78% vs. 51%).
The article is long and detailed; I recommend the full read including some helpful tables, with references to the major studies, and charts.
In concluding, the author, who admits receiving grant support from Amersham Health (a GE subsidiary), consulting fees from Bayer and lecture fees from AstraZeneca, returns to the hypothetical patient, and what might be said to a woman in her 40s who lacks an outstanding risk (such as a genetic disposition or strong family history):
…Mammography screening every 2 years will find two out of every three cancers in women her age, reduce her risk of death from breast cancer by 15%. There’s about a 40% chance that further imaging (such as a sonogram) will be recommended, and a 3% chance for biopsy with a benign finding.…
In my opinion (ES) this is key – that the chances of a false positive leading to biopsy are only 3% for a woman in her 40s. If those biopsies are done in the radiology suite with a core needle, every 2 years for women of average risk, the costs of false positives can be minimized.
About the author…Dr. Elaine Schattner is a trained oncologist, hematologist, educator and journalist who writes about medicine. Her views on health care are informed by her experiences as a patient with scoliosis since childhood and other conditions including breast cancer. Elaine is a Clinical Associate Professor of Medicine at Weill Cornell Medical College in New York City where she teaches part-time. Her blog, Medical Lessons, is geared towards dissecting and providing commentary on how healthcare news is comunicated in order to foster learning and help bridge the gap between patients and doctors.