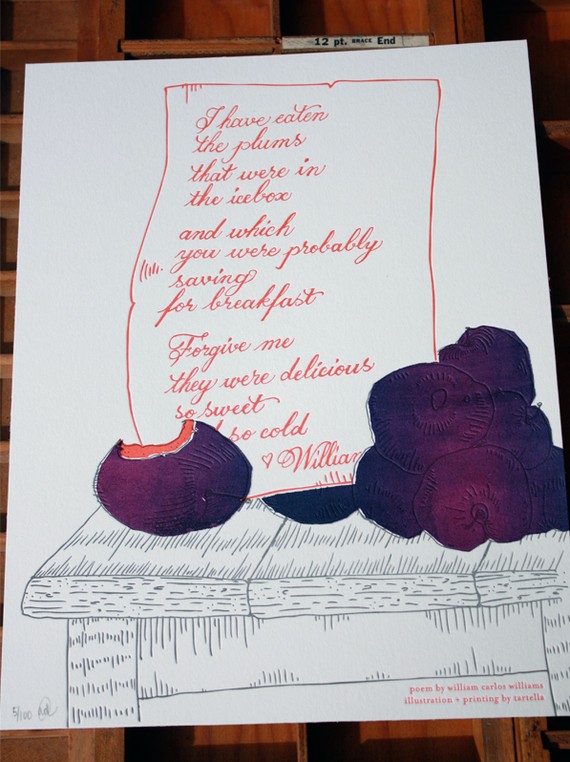
Plums…delicious, sweet. And, good for bone health?
[Image: all rights reserved 2012. Used with permission by Tartella. Visit them online at http://www.tartella.com/ and if you love this print as much as I do, you can purchase it in their Etsy store.]
Yowza! I am excited about study findings published in the British Journal of Nutrition linking dried plums (better known as the lowly prune) to improved bone mineral density in menopausal women. If these findings ring true and can be duplicated in larger groups of women, they may have a tremendous impact on the steps we take to preserve our bones as we age — most notably, the ability to avoid bisphosphonates — which have been linked to collapse of jaw bones and even an increase in the fractures they are supposed to protect. Moreover, although calcium supplementation is broadly recommended, there is an indication that it may increase heart disease risk in some women.
However, as one of the investigators note in BJN, study findings consistently show that greater intakes of fruits and vegetables have positive effects on bone resorption (the breakdown of bone), adding prunes among fruits and onions among vegetables, to be the most effective functional foods in terms of their actions on modulating the process by which bones break down and build up again.
In animal studies, prunes were shown to prevent bone loss as well as restore bone mineral density in conditions created to mimic bone loss associated with osteoporosis. In addition to these studies, researchers had also a conducted a short, three-month study in menopausal women in whom bone mass was improved simply by eating around 10 prunes (100 g) daily.
In this latest iteration, the same researchers compared two groups of menopausal women assigned to eat around 100 gm of prunes (~10) or 75 gm dried apples (the equivalent of the prunes in terms of energy, carbohydrates, fats and fiber) daily for a year. All of the women had been in menopause for anywhere from one to 10 years, were not on hormone therapy and were also asked to take 500 mg calcium plus 400 IU vitamin D with their daily dried fruit.
The findings? By the end of one year, women eating prunes had significantly lower levels of several markers for bone turnover compared to their peers who ate dried apple. Conversely, the prune eaters had significantly higher levels of bone mineral density in their ulnas (one of two long bones in the forearm) and spine compared to the other group. The researchers say that this is partly due to the fact that prunes suppress the rate at which bone cells break down bone, which exceeds the rate at which they build it up as we age.
Women in particular lose up to 50% of their spongy, or trabecular bone (the network that makes up most of bone structure) and up to 30% of their cortical bone (the outer shell) within the first 10 years of the onset of menopause. Of the investigators, Professor and chair of Florida State University’s Department of Nutrition, Bahram Arjmandi, suggests that women (and men) interested in maintaining or even improving bone health start eating two to three prunes a day and gradually build to six to 10. Arjmandi says to “do something meaningful and practical beforehand, ” and “don’t wait until you get a fracture or are diagnosed with osteoporosis” and need medication.
Sure, prunes get a bad rap. But aren’t ‘bad’ bones even worse? Truly, prunes can be ‘as delicious and sweet’ as plums. The writing on the wall suggests that you don’t wait until it’s too late.
Read More
Wednesday Bubble: is there a connection between dry mouth and osteoporosis?
This week’s bubble is neither burstable or good news. But it is important:
Dry mouth and bone mineral density appear to be related.
Say what?!!!
A bit of background is needed…
Osteoporosis is fast becoming a major health problem and as I’ve written time and again on this blog, is a significant characteristic of menopause, namely as the result of waning estrogen levels that lead to an imbalance between the build up and turnover of bone cells. Parathyroid hormone and cortisol have also been linked to bone turnover.
Dry mouth (i.e. a feeling of dryness in the mouth and need to use liquids while eating) and burning mouth syndrome (i.e. burning in the tongue or oral mucus membranes and taste alterations) are also common during menopause, affecting up to 40% of women. Until now, experts have not been able to adequately determine why these symptoms occur and more importantly, effective management strategies.
The link? Recent data have shown that estrogen levels may be significantly lower and both parathyroid and cortisol levels significantly higher in menopausal women who complain of dry mouth. Moreover, as the results of a new study in Menopause show, there may be a true relationship between these two conditions and that bone loss may be the actual cause of oral dryness and related symptoms. In this study, researchers evaluated 60 women in menopause (mean age 56) for the presence and severity of dry mouth and then based on their results, divided them into two groups. Dry mouth was confirmed by responses to a scientific questionnaire and collections of saliva. The researchers also measured bone mineral density at the spine.
Importantly, the participants were not particularly active and none engaged in any sports activity, except walking. The women were also matched by body mass index, age, or years of menopause. And yet, women with low bone mineral density, including relationship to other women in the same age group and 30 years younger, were significantly more likely to experience dry mouth and had significantly less saliva when their appetites were not stimulated.
Clearly, more research is needed. However, there are some things you can do now. The first strategy to combat osteoporosis and bone loss is to get measured for bone loss and disease markers. Steps like calcium supplementation, a healthy diet and regular exercise are critical. And if you suffer from dry mouth? You may want to speak to your dentist about a referral for a bone mineral density scan or better yet, have him or her contact your gynecologist or regular health practitioner for a pow wow. Not only may you help your bones, but you may actually change that dry feeling.
Read MoreNo bones about it: the best things in life are sea
Did you know that eating fish that live in the sea might help boost bone health and density? Although most of the attention on the link between osteoporosis and diet has focused on calcium, milk and soy, a few studies suggest that other nutrients, such as polyunsaturated fatty acids and omega-3s, may also play a role.
According to novel research published in the journal Osteoporosis International, a greater intake of sea fish, but not shellfish or freshwater fish, is linked to as much as almost a 7% increase in bone-mineral density and an almost 10% increase in bone mass in general and in the hip areas in particular. On average, the women studied, all of whom were menopausal, were eating about .8 ounces of sea fish a day — about 16% of their total daily protein intake, and about 2 ounces daily of sea fish and shellfish combined. Factors like body weight, smoking, and alcohol did not appear to influence the association between fish from the sea and bone benefits. (Note – the study did not specifically address the exact types of fish that they women were eating other than to say, it wasn’t freshwater or shellfish.)
Interestingly, prior studies have found similar links between higher bone mineral density and a high consumption of seafood among menopausal women. Researchers say that a higher intake of fish versus animal protein or low quality foods may account, at least in part, for the higher bone mass.And while they are unable to offer any reasonable explanation for why sea fish, especially the oily types like salmon or mackerel or tuna benefit bone health while freshwater fish does not, they say that it might be due to the high level of vitamin D , which has long been associated with favorable bone mass. Omega-3 fatty acids are also thought to play important roles.
The take-away on this is to eat more fish from the sea. Clearly, environmental concerns, like overfishing and high level of mercury, may influence your seafood selection, however, Seafood Watch offers some great resources how to make safe and careful choices. What I love about this information is that it not only serves to encourage healthier eating, which can help keep those pounds away (My friend Danielle Omar wrote a great guest post about sea veggies and weight about a month ago), but also provides another strategy for keeping bones healthy as we age. Yup, the best things in life are sea.
Read MoreOsteoporosis: what’s the 411?
Osteoporosis and low bone mineral density are well-known issues for menopausal women. As women enter the early stages of menopause, their bones lose their ability to retain their mass and manufacture new bone tissue, resulting in bone loss and increasing the risk for osteoporosis and its deleterious effects. What’s more, experts estimate that by the time a woman reaches the age of 50, she has a 40% risk of suffering a fracture due to osteoporosis for the rest of her lifetime. Besides the discomfort, hip fractures in women lead to a loss of mobility, a need for long-term care and even death. No bones about it; osteoporosis is no laughing matter.
Risk factors that contribute to a loss of bone mineral density are varied and include age, genetics, low calcium/vitamin D intake, body weight and menopause status. However, osteoporosis is a mixed bag and there are several underlying conditions that can also contribute to its severity:
- Medications (e.g. heparin, anticonvulsants, progesterone, chemotherapy agents)
- Parathyroid hormone (which regulates how calcium is used in the body – released in urine, absorbed in diet and stored in bones)
- Calcium imbalance due to excessive calcium excretion, aka “hypercalciuria,” Vitamin D deficiencies
Before I move into the land of boredom, there is a reason why I’m sharing some of the facts about osteoporosis, which BTW are readily available on the National Osteoporosis Foundation website (if you’ve not perused the site, I strongly encourage you to do so!): there is an indication that your practitioner might not be looking for these important secondary causes! Moreover, sometimes they are not even readily apparent.
Writing in the journal Menopause, researchers studying 204 menopausal women say that they’ve discovered that among the various factors that influence a woman’s risk for low bone density, several impact severity:
- Low vitamin D levels (82% of women in this study had below optimal levels)
- Elevated parathyroid hormone levels (35% of women in the study) — (leads to too much calcium in the blood and a loss of calcium from bones)
- Unusually high calcium excretion (20% of women in the study)
- High bone turnover rates (41% of women in the study) — (high bone turnover refers to an increase in the breakdown, or resorption of bone without a compensation for the repair of bone, leading to compromised strength, thinning, brittleness and fractures)
There are a number of dietary and lifestyle strategies to prevent osteoporosis, including incorporating Vitamin D and calcium supplementation, omega-3 and omega-6 fatty acids into the diet, and increasing physical activity. More recent findings suggest that beer, onions and even flaxseed may be effective (although more research is needed). Meanwhile, if you’ve recently learnt that your bone mineral density is low (or that you’ve actually developed osteoporosis) you need to speak to your practitioner about some of these other markers. Knowledge is power and the more you know, the greater the likelihood that you can start incorporating treatment now to prevent further bone deterioration.
That’s the 411. No bones about it!
Read MoreHip fracture, early menopause and age

Good news for you early menopausers: Australian researchers say that early menopause does not increase the risk for hip fractures due to weaker/lower bone density.
Bone density or bone mineral density (BMD) refers to the individual strength of bones, generally in relation to their calcium content. BMD is known to decline rapidly during the time period that immediately follows menopause, leading to osteoporosis and hip fractures. Because there have been lingering questions regarding how early menopause influences fracture risk, researchers decided to undertake a study that would sort out the relationship of age, menopausal status and age at menopause to hip fractures. Over 561,000 pre-, peri- and postmenopausal women who had never used hormone replacement therapy participated in the study (which lasted, on average, 6 years).
They found that hip fractures were about twice as likely in postmenopausal versus premenopausal women. But more importantly, when age was factored in, this relationship dropped out. In fact, rates of hip factors was as much as seven times higher among women who were between the ages of 70 and 74 compared to women between the ages of 50 and 54. What’s more, age at menopause had little effect on fracture risk.
What you can do now…..
- Calcium – OHC is a formulation that has recently been shown to impart greater protection against bone loss than calcium carbonate.
- Isoflavones – Here, type/source may be important.
- Exercise – Including weight bearing, resistance and strength-training.
Meanwhile, if you are in early menopause, here’s one risk you don’t have to worry about. It’s no reason not to take preventive measures to prevent bone loss in older age. But it is a reason to breathe a bit easier.
Read More