Wednesday Bubble: is DHEA the path towards a better sex life?
Today’s Bubble is a doozie that can one of two ways: in the yes(!) column or in the no (!) column. I’ll leave it to you to decide.
DHEA is the most abundant sex hormone in circulation and is mostly secreted by the adrenal glands. Research has shown that low DHEA levels in pre- and postmenopausal women may negatively affect sexual functioning, while ample blood levels may enhance sexual functioning, cognitive functioning and wellbeing. Yet, whether or not DHEA really works continues to be controversial. And the reason behind the burgeoning interest is the quest to find a suitable replacement for HRT. The thing is? There are lots of suitable, evidence-based replacements that are not broadly accepted by many medical professionals and many of these are discussed regularly on this blog. Nevertheless, here’s what researchers have just discovered about DHEA.
The researchers, from Pisa, Italy, followed 48 healthy, postmenopausal women for a year. During this time, they divided 36 women who were experiencing troublesome menopausal symptoms and requesting hormone replacement into three groups:
- 12 women who received 10 mg daily of DHEA
- 12 women who were given combined HRT
- 12 women who received the synthetic hormone, tibolone, daily
The fourth group was comprised of 12 women who did not wish to use HRT. They received daily vitamin D (400 IU) and calcium to help combat osteoporosis.
At the start of the study, all of the women reported similar sexual activity. However, after a year of treatment, women taking DHEA had significant increases in sexual interest and activity scoring almost 14 points higher on a questionnaire used to measure sexual interest, satisfaction, vaginal lubrication, orgasm and sexual partner. The women taking HRT experienced similar benefits, and women in both of these groups reported engaging in more sexual intercourse compared to women taking Vitamin D and calcium. Women taking the synthetic hormone also had increased sexual interest scores but they were not as high as the other two hormone groups. The magnitude of improvements in menopausal symptoms was also similar between the DHEA, HRT and tibolone groups.
The reason for this improvement appears to be the effect that DHEA has in terms of improving blood levels of the hormones estradiol and progesterone, both of which decline during menopause. It also appears to positively affect adrenal functioning.
What to think? Well, the study didn’t include any information on side effects. This is what Mayo Clinic has to say in that regard:
“No studies on the long-term effects of DHEA have been conducted. DHEA can cause higher than normal levels of androgens and estrogens in the body, and theoretically may increase the risk of prostate, breast, ovarian, and other hormone-sensitive cancers. Therefore, it is not recommended for regular use without supervision by a licensed health professional.”
Another important fact, acknowledged by the researchers, is that DHEA was only studied in 12 women, hardly enough to draw any firm conclusions. But they do believe that the findings, albeit preliminary, are encouraging, especially for women who “may have problems in taking more conventional HRT.”
Personally, I believe that it’s waaaaay too early to even consider DHEA as an alternative to HRT and in particular, to androgen therapy for sexual health. I want to see more information on side effects before it’s even on the radar. Meanwhile, I would love to hear what you think:
Yes!?
or,
No!?
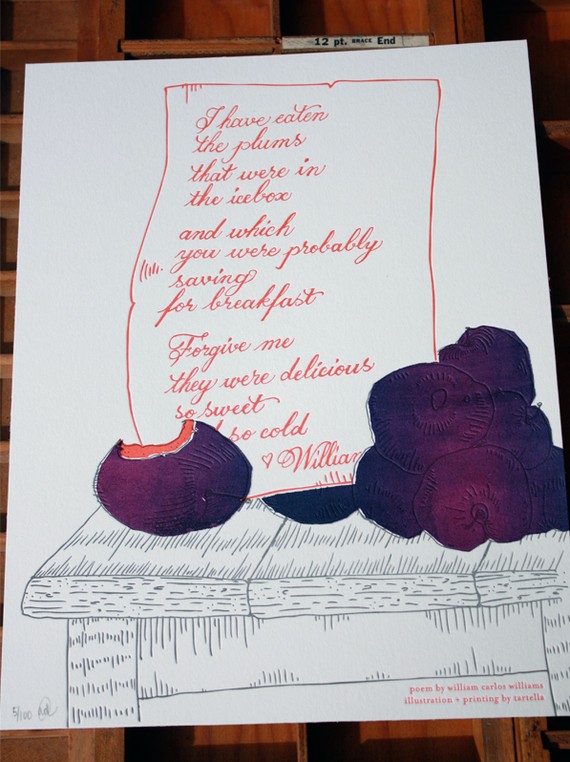
Read MorePlums…delicious, sweet. And, good for bone health?
[Image: all rights reserved 2012. Used with permission by Tartella. Visit them online at http://www.tartella.com/ and if you love this print as much as I do, you can purchase it in their Etsy store.]
Yowza! I am excited about study findings published in the British Journal of Nutrition linking dried plums (better known as the lowly prune) to improved bone mineral density in menopausal women. If these findings ring true and can be duplicated in larger groups of women, they may have a tremendous impact on the steps we take to preserve our bones as we age — most notably, the ability to avoid bisphosphonates — which have been linked to collapse of jaw bones and even an increase in the fractures they are supposed to protect. Moreover, although calcium supplementation is broadly recommended, there is an indication that it may increase heart disease risk in some women.
However, as one of the investigators note in BJN, study findings consistently show that greater intakes of fruits and vegetables have positive effects on bone resorption (the breakdown of bone), adding prunes among fruits and onions among vegetables, to be the most effective functional foods in terms of their actions on modulating the process by which bones break down and build up again.
In animal studies, prunes were shown to prevent bone loss as well as restore bone mineral density in conditions created to mimic bone loss associated with osteoporosis. In addition to these studies, researchers had also a conducted a short, three-month study in menopausal women in whom bone mass was improved simply by eating around 10 prunes (100 g) daily.
In this latest iteration, the same researchers compared two groups of menopausal women assigned to eat around 100 gm of prunes (~10) or 75 gm dried apples (the equivalent of the prunes in terms of energy, carbohydrates, fats and fiber) daily for a year. All of the women had been in menopause for anywhere from one to 10 years, were not on hormone therapy and were also asked to take 500 mg calcium plus 400 IU vitamin D with their daily dried fruit.
The findings? By the end of one year, women eating prunes had significantly lower levels of several markers for bone turnover compared to their peers who ate dried apple. Conversely, the prune eaters had significantly higher levels of bone mineral density in their ulnas (one of two long bones in the forearm) and spine compared to the other group. The researchers say that this is partly due to the fact that prunes suppress the rate at which bone cells break down bone, which exceeds the rate at which they build it up as we age.
Women in particular lose up to 50% of their spongy, or trabecular bone (the network that makes up most of bone structure) and up to 30% of their cortical bone (the outer shell) within the first 10 years of the onset of menopause. Of the investigators, Professor and chair of Florida State University’s Department of Nutrition, Bahram Arjmandi, suggests that women (and men) interested in maintaining or even improving bone health start eating two to three prunes a day and gradually build to six to 10. Arjmandi says to “do something meaningful and practical beforehand, ” and “don’t wait until you get a fracture or are diagnosed with osteoporosis” and need medication.
Sure, prunes get a bad rap. But aren’t ‘bad’ bones even worse? Truly, prunes can be ‘as delicious and sweet’ as plums. The writing on the wall suggests that you don’t wait until it’s too late.
Read More
Your bone health: the role of diet
Osteoporosis. That scary condition that can result in bone fracture in up to 40% of US women after the age of 50. In the UK, it’s been estimated at least half of women over age fifty will have some sort of osteoporotic fracture. So it’s truly no laughing matter.
I’ve tried to cover osteoporosis extensively since starting Flashfree and you can find many of those posts here. However, I am especially intrigued by novel research that demonstrates that dietary pattern, that is, particular combinations of foods that we eat, may influence bone turnover, a term used to describe the balance between bone formation and bone loss (a process that goes on constantly through our lives) resulting in a net loss or gain in bone tissue. Moreover, dietary pattern may also specifically influence bone resorption, i.e., the process by which cells called osteoclasts break down bone so that minerals (like calcium) can be released into the bloodstream.
The researchers, who studied 3,236 postmenopausal women between the ages of 50 and 59, say that to date, most research has focused on link between specific nutrients and bone health, nutrients such as vitamin D or calcium. However, they point out that most individuals eat a variety of foods the contain combinations of nutrients. Therefore, they believed that there might be value in actually examining how the whole diet and the presence or absence of certain nutrients, affects the skeleton.
Consequently, they took initial body mass index measures, bone mineral density measures, assessed dietary habits by consumption of 98 foods, how often they were consumed and by portion size, and then, based on evaluation of how often these foods were consumed by the participants, further characterized them as the following dietary patterns: “healthy,” “processed,” “bread/butter,” “fish and chips” (the study took place in Scotland!) and “snack food.”
Overall, the women in the study actually consumed a large proportion of fruits and vegetables and on average, at least three cups of tea daily. Bread and potatoes tended to comprise the greatest source (at least percentage-wise) of “energy” to the diet. To a lesser extent, yogurt, cream, fats, oils, biscuits and milk also contributed a substantial amount of energy to the diet. However:
- Of the five types of dietary patterns, a healthy diet was most associated with better bone health, and specifically, a reduction in bone resorption. Specific foods included fruits and vegetables, white meat, white and oily fish and dairy, all nutrients that have been previously associated with beneficial bone health.This combination of foods also provided adequate protein.
- Conversely, eating mainly a ‘processed foods’ (i.e. cereal, processed meats, cake, desserts, dried fruits, soup, bread, and fats and oils) diet, and a “snack foods” diet (i.e. candy/cookies, potato chips, sauces) were both associated with reductions in bone mineral density.
- The results didn’t change when factors, such as whether or not women were taking drugs to fight osteoporosis, were taken into account.
The bottom line is that when it comes to bone health, it’s important to eat healthy, pack your diet with fruits and vegetables, and stay away from junk and processed foods. Focus on foods that are risk in calcium and balanced levels of good protein. Although this may seem intuitive, the findings emphasize that a poor diet may ultimately result in poor bone health and increase fracture risk as you age.
Time to restock the fridge? No bones about it!
Read MoreThe Roundup – a few highlights
[Credit: Special thanks to artist Darryl Willison of whimsicalwest.com. Please visit his site and support his work.]
I would be remiss if I didn’t admit that this well-received monthly feature seems to have fallen off Flashfree post list. So, as of today, I am officially reviving it. Rather than list four month’s worth of highlights, I’ve decided to pick and choose a few favourites so you don’t miss anything. Still, my mind isn’t yours’ so feel free to peruse the monthly archives.
Without further ado…
- Female viagra hits a new low in the bedroom. Hypoactive sexual desire disorder is real to many women, who suffering from reduced libido and interest. But can a pill address the underlying issues, such as emotions, relationships, environment and hormones?
- HRT – Wait a moment! Stopping hormone replacement might be bad for your menopause. In fact, it appears that symptoms might suddenly appear out of nowhere.
- When it comes to calcium, think moderation. Women need calcium and vitamin D as they age. But too much of a good thing may be dangerous.
- That ole glass ceiling still isn’t cracked. Want a raise? Some individuals would have you believe that you should let your femininity drive your bargaining.
- HRT – Ask the hard questions. Are you considering starting hormone replacement? Be sure that you know the facts.
- It’s about time…weight, that is. The time of day may determine how much weight you gain as much as what you are eating.
When it comes to calcium, think moderation
There’s a new condition emerging among postmenopausal women: calcium alkali syndrome (milk-alkali syndrome).
Milk calcium what?!
A wonderful commentary slated to appear online this month in the Journal of the American Society of Nephrology highlights the dangers of consuming too much calcium . In it, the author tells the tale of Chicago bartender Bertram Welton Sippy, who in 1915, introduced his bar patrons with ulcers to the Sippy diet, hourly intake of milk, cream eggs and farina cereal interspersed with Sippy powders on the half hour (i.e. dissolvable antacid like minerals that included calcinated magnesia, sodium bicarbonate and bismuth subcarbonate). A recipe for disaster? You bet, because the overkill of calcium and minerals led to symptoms that include headache, nausea, vomiting, mental clouding, a distaste for milk and eventually, kidney failure. Yikes!
While men were the primary victims of the condition in the last century, it appears that a new group of victims started to emerge in the 90s – postmenopausal women who have increased their intake of calcium and vitamin D to combat osteoporosis. And although calcium, not milk, is the primary driver, the condition is the third most common cause of hospital admission for significantly elevated blood calcium levels.
It appears that the necessity to preserve our bones has created a modern version of the Sippy diet.
The best strategy for reducing the risk of calcium-alkali syndrome is to moderate your intake of calcium supplements. In fact, the authors say that although an average of more than 4 g/day of supplemental calcium is most commonly linked to illness, small numbers of women have developed it on as little as 1 to 1.5 g calcium a day. Of note, while younger adults are able to store excess calcium in bone, aging seems to reduce this natural defense and instead, calcium tends to leave the bone (thereby leaving us more susceptible to fragile bones and osteoporosis) and in turn, a potential build up in the bloodstream. Still, the authors emphasize that calcium supplements in moderation are a necessary and beneficial option for women at risk for osteoporosis. The trick is to limit supplemental calcium intake to no more than 1.2 to 1.5 grams daily because our bones need protection. Read the label. And speak to your healthcare practitioner. When it comes to protecting our bones through supplementation, moderation appears to be the key.
p.s. Stay away from the Sippy diet. It’s a sippier slope (sorry, couldn’t resist!).
Read More