Wednesday Bubble: Depressed? It may be high testosterone
As I’ve written previously, depression and hormonal imbalance go hand in hand as much as love and marriage, babies and carriages, and yin and yang. As many as 40% of women are affected by depression during menopause, but there are other factors that come into play, including gender (women are 1.5 to 3 times likelier than men to report a lifetime history of depression), stress, family life, general health issues, a lack of exercise and genetics. Moreover, research has shown that how women perceive the effect of menopause and its symptoms on their physical health can significantly affect whether or not they develop depression at the start of the ‘pause.
I’ve got one more factor to add to the mix: testosterone. Findings reported at this week’s International Federation of Fertility Societies/American Society for Reproductive Medicine meeting suggest that when it comes to depression in menopause, high testosterone levels may be at-play, at least in Caucasian women.
Among 400 women studied over 14 years (who were 35 to 47 when the study began), 76% had a history of depression. Still, researchers say that this history did not appear to affect the relationship between high testosterone levels and depression scores; in fact, Caucasian women with the highest testosterone levels were 27% more likely to have depression than women who had the lowest levels. In fact, when considered in totality, each jump to the next measure of testosterone levels (four in all) increased the risk of depression by 14%.
Importantly, the researchers did not see the same increase in depression among African-American women. Rather, African-American women with the highest testosterone levels were 26% less like to have depression.
There is no indication of the reasons why testosterone affects mood in Caucasian versus African-American women. However, it’s important that we have another piece of the puzzle. Take note: if testosterone patches ever make it to market in the U.S., women with preexisting depression may want to step back before hopping on that bandwagon.
Read MoreSleep and the ‘pause: valerian and lemon balm?
 Here’s a sobering thought: by the year 2030, over one billion women worldwide will be affected by menopausal symptoms, and that number is projected to increase by 47 million women annually. Sleep issues, namely disruption in sleep patterns caused by hormones, stress, hot flashes, night sweats and aches and pains affect roughly 81% to 83% of women in menopause. Of these, more than half report insomnia.
Here’s a sobering thought: by the year 2030, over one billion women worldwide will be affected by menopausal symptoms, and that number is projected to increase by 47 million women annually. Sleep issues, namely disruption in sleep patterns caused by hormones, stress, hot flashes, night sweats and aches and pains affect roughly 81% to 83% of women in menopause. Of these, more than half report insomnia.
If you do the math, the sleep issue suddenly becomes very, very big!
Short of going the prescription route, there are a variety of strategies that reportedly help. You can read about some of those here. And, I’m happy to add one more: valerian/lemon balm.
Valerian is an herb used in variety of forms since the time of Ancient Greece. Its use in insomnia was first reported in the second century and it was even used during WWII to alleviate stress during air raids. Today, it is widely used for stress and sleep issues. While few adverse effects are associated with valerian, it may interact with benzodiazepines (e.g. xanax), barbituates or drugs that suppress the central nervous system (morphine, propofol); caution is also advised if you are taking St. John’s Wort, kava and melatonin.
Lemon balm also has a long history in traditional medicine, and as long ago as the middle ages, was used to combat stress and anxiety, promote sleep and calm nerves. While it is relatively benign, experts say that caution should be used if you are also taking sedatives or thyroid medications, or antiretroviral agents.
A few safety issues aside, the combination of the two is potentially explosive! According to new study findings, a combination — 160 mg valerian/80 mg lemon balm — in capsule form significantly improved sleep quality, patterns of sleep and sleep duration in women experiencing menopause symptoms by as much as 36%. In fact, over a month one month period, these improvements were as much as 28% higher than findings in women taking placebo capsules. What’s more, the amount of valerian used in the capsule was more than two- to four-fold lower than doses traditionally used in sleep studies demonstrating significant sleep quality improvements; this speaks to the addition of lemon balm. Additionally, the benefits appear to occur without side effects; no adverse effects were reported.
Sleep and the ‘pause….valerian and lemon balm might just do the trick!
Read MoreAre you a snackaholic?
I don’t know about you when the stress levels accelerate or the weather starts to get nippy, I feel more inclined to snack. It appears that I am not alone; according to a study published online in the European Journal of Clinical Nutrition, 97% of adults report consuming at least one snack a day. Not only has snacking become common practice, but people snack more often and the snacks themselves are larger than ever. Supersize that snack! Yikes!
Fortunately, the next time a craving hits, there may be a better option than a bag of chips: almonds. In fact, Purdue University researchers report that eating 1.5 ounces daily of dry-roasted, lightly salted almonds may reduce hunger without affecting body weight.
I bet that you thought that nuts are fattening, right?
To test the almond theory, the researchers asked a group of 137 adults to:
- Avoid all nuts and seeds
- Consume 1.5 ounces of almonds daily with either breakfast or lunch
- Eat 1.5 ounces of almonds daily in between either breakfast or lunch (i.e. within two hours of the last meal and at least two hours before the next meal)
Other than the inclusion or exclusion of almonds at a defined time, all participants followed usual eating and physical activity patterns. They also met with a nurse weekly to record weight and dietary habits and discuss sensations of hunger , fullness or desire to eat. Additionally, at various benchmarks throughout the four weeks that the study took place, blood and blood sugar information were calculated.
Here’s the interesting part: despite an additional 250 calories a day from an almond snack, none of the adults participating in the study increased the total number of calories they consumed in a day or gained weight over the four week study. Additionally, eating almonds as a snack rather than part of a meal or avoiding them altogether appeared to significantly suppress hunger or the desire to snack. Another benefit gleaned from eating an almond snack was an improvement in overall vitamin E and monounsaturated fat profiles, which respectively, can help protect cells from damage and promote better absorption of nutrients from the foods that we eat, as well as improve heart health.
Mind you, conclusions can only be made with regard to the short term benefits of almonds. But in so far as snacking? Almonds may be the optimal snack, increasing a sense of fullness, decreasing caloric intake and counteracting the constant snacking desire, all without increasing overall weight. Craving a nibble? Reach for a handful of almonds.
Read More
Wednesday Bubble: Evolution?
Do they or don’t they? Inquiring minds want to know!
Tell me what your flashes are like and how they’ve been as you’ve been moving through the ‘pause. Hopefully, we can collectively come up with some effective solutions!
Read MoreBreast Cancer & Physical Activity: What’s the 4-11?
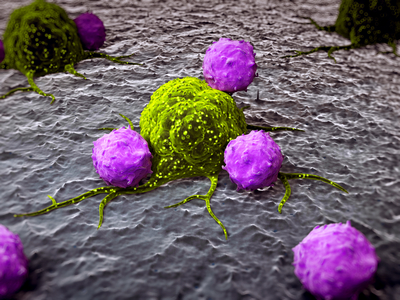 Want to reduce your breast cancer risk? According to new study findings published in Cancer, Epidemiology, Biomarkers & Prevention, at least an hour of moderate to vigorous daily activity may significantly reduce breast cancer risk in postmenopausal women. That’s just an hour a day or at least seven hours a week.
Want to reduce your breast cancer risk? According to new study findings published in Cancer, Epidemiology, Biomarkers & Prevention, at least an hour of moderate to vigorous daily activity may significantly reduce breast cancer risk in postmenopausal women. That’s just an hour a day or at least seven hours a week.
However, is it really that simple? Moreover, are there other factors at play that influence risk such as hormone receptor status, body mass index, weight gain or use of postmenopausal hormones? Notably, all of these have been linked with an increased cancer risk.
Indeed, when the researchers evaluated information provided by over 73,000 women (ages 50-74) over a course of 12 years, they were able to confirm what has eluded medical science for years: even moderate intensity activity, i.e. walking, when conducted daily, can have a major impact on breast cancer risk. Participants were asked to report, via questionnaire, the average number of hours they spent walking, jogging, running, lap swimming, tennis/raquetball, bicycling, doing aerobics or calisthenics and dancing. Assessments were also made on the number of MET hours — metabolic equivalent hours — were expended. Finally, adjustments were made to the findings that accounted for possible confounding factors, things like education, adult weight change and BMI, smoking and alcohol, age at menopause, personal history of breast cysts, hysterectomy or oopherorectomy, family history of breast cancer and finally, use of any type of hormone therapy and if use was current.
On average, women expended 9.5 MET-hours/week, which is equivalent to 3.5 hours/week of moderately paced walking. Additionally, 47% reported that walking was the only recreational physical activity that they participated in. Overall, these women tended to be leaner, more likely to lose or maintain their weight, more likely to drink alcohol and less likely to be current smokers. Importantly, they were less likely to use hormone replacement. And, compared to more vigorous physical activity (>42 MET-hours/week), women who reported walking at least an hour day were found to have a 14% lower risk for breast cancer; their more active peers almost double this – or a 25% lower risk. These findings remained even after the researchers made adjustments for the factors mentioned above – body type, hormonal status and estrogen receptor status.
In a related press release, a senior epidemiologist with the American Association for Cancer Research and a study co-author, Dr. Alpa Patel, points out that “current guidelines recommend that adults should strive to get at least 2.5 hours per week of moderate intensity activity or 75 minutes per week of vigorous intensity activity for overall health.” Yet, less than half of U.S. American women are active at these levels and the researchers note that an even smaller proportion are likely to achieve the higher levels necessary for breast cancer reduction. And yet, just an hour a day of moderate intensity walking can have a positive impact.
I cannot stress this enough: get off of your butts and walk. It doesn’t take a gym membership or a major equipment investment. And, it may actually prevent breast cancer!
Read More
Newsflash: HRT, a “complex pattern of risks and benefits”
I’m not sure if you saw the headlines yesterday in light of news on the government shutdown but the healthwebz are buzzing about a study published in published in JAMA evaluating outcomes in the now infamous Women’s Health Initiative and the utilization of hormone replacement therapy (HRT) for menopausal symptoms. My only question is why do we keep beating this dead horse?
However, I would be remiss if I did not share the highlights of this latest analysis. So here’s what you need to know and honestly, it’s not very different than the stance of other organizations:
- The study or analysis, if you will, provides a detailed overview of the findings from both the original and extension trials of the WHI, looking at both combination and estrogen alone hormone therapy.
- Overall, the risks of combination therapy appear to have outweighed the benefits during the trial. During the extension period, the risk for heart disease remained elevated, a reduced risk for endometrial cancer was seen. Among women who had had hysterectomies before taking HRT, a more balanced risk/benefit equation was seen.
- With regard to breast cancer, the risks of taking combination therapy versus estrogen alone are not equal; more women have adverse effects from combination therapy.
- Proponents of HRT have long argued that age matters. The researchers involved in this analysis state that age influences the effects of hormone therapy ‘in some cases’ as does time since menopause onset, and that results appear to be better for younger versus older women, at least in terms of overall death rates due to all causes, deaths due to heart attack and deaths due to cancer.
- HRT appears to have a more harmful effect on coronary heart disease when used in older women; the effect on younger women is unclear. They say that further research is needed.
- Less clear is the link to breast cancer. While the researchers acknowledge that combined hormones may increase breast cancer incidence and cancer is diagnosed at a later stage, the risk might decline once HRT is stopped. They hypothesize that the progestin component is at play but say that more research is needed.
- While combined HRT may reduce endometrial cancer, it might also increase ovarian cancer risk, as may estrogen alone.
- Combined HRT has been shown to increase deaths from lung cancer, although neither combined or single hormone therapy appears to influence the total incidence of the cancer.
- With regard to diabetes, clot risk, gall bladder disease and dementia? A decrease in diabetes risk during treatment disappears overtime and the risk for clotting and gallbladder disease as well as dementia increase.
The researchers write that the overall findings do not support the use of either combination therapy or estrogen alone for chronic disease prevention, even in younger women. And they note that the risks of combination HRT outweigh the benefits, irrespective of a woman’s age.
Look, I don’t need to cover any additional findings or conclusions. Combination HRT is not all it’s cracked up to be. Speak to your doctor. Analyze your risks and determine if a fewer hot flashes or mood swings are worth it. Only you can decide. Me? I’m sticking with the devil I know and like: alternative strategies.
Read More
Alternative medicine and the ‘pause: what your gynecologist is thinking
Women rank among the highest consumers of complementary and alternative medicine for their healthcare, and according to the National Center for Complementary and Alternative Medicine, age matters. In fact, the largest percentage of adults reporting that they use alternative medicine strategies are 50 to 59 years old, and as many as 42% discuss their use with their doctors. However, what does your gynecologist think about complementary and alternative medicine use? Is she or he supportive and what modalities tend to rank highest in terms of recommendations or endorsements? Moreover, how do gynecologists differ in their opinions?
In the U.S., most ob/gyns appear to believe that convention medicine practices for reproductive issues might benefit by the integration of complementary strategies. However, most of the positive beliefs focus on biofeedback, chiropractic, acupuncture or meditation. Conversely, the doctors report that they would not recommend dietary changes or Traditional Chinese Medicine and a majority were not strong supporters of herbal medicine. This is in direct conflict with German gynecologists. But why should we care about the Germans and what they think!!!?
To digress, I don’t know how many of you are familiar with the Commission E Monographs but, they comprise the world’s leading scientific summaries on the use of medicinal herbs in health and disease. In the late 1970s, the German Ministry of Health established Commission E, a panel of experts charged with evaluating the safety and efficacy of the herbs available in pharmacies for general use. In all, the group published 380 herbal monographs that are considered “the most accurate information available in the entire world on the safety and efficacy of herbs and phytomedicines.” Hence, the Germans definitely have a leg up when it comes to alternative medicine, at least when it comes to the use of herbal alternatives.
So, let’s take a look at a similar survey experience newly published in Complementary Therapies in Medicine, in which over 2,500 respondents indicated a familiarity with the use of alternative medicine specifically for menopausal symptoms. Almost all of the gynecologists had some experience with black cohosh, chaste tree berry and St. John’s Wort and believed them to be effective. And the modality that they felt was most effective? Lifestyle changes and alteration (think: change in dietary habits, physical activity, reduction of stress, etc). The least effective strategies, at least in the eyes of German doctors, were yoga, acupuncture and homeopathy.
The researchers point out that the viewpoint of German doctors is important because these practitioners play an important and consistent role counseling women who complain of menopausal symptoms. The same is true for their U.S. counterparts. And yet, despite the wealth of data in the Commission E monographs, many doctors still continue to question effectiveness and scientific evidence supporting the use of alternatives.
Will this make a difference with regard to the choices that women are making? Probably not, because as I’ve been writing for years, one size does not fit all, especially when it comes to weighing the benefits versus the risks of hormone replacement.
The next time you have your annual with your gynecologist, find out what she or he thinks of complementary and alternative and strategies and most of all, ask why. What she or he is thinking might not be aligned with what you find works best for you.
Read More











