She works harder for the money
Awhile back, I wrote a post about how menopause impacts our occupational health and the need for greater awareness among managers of the types of health challenges that their middle aged female employees might be going through. This issue is evidently an ongoing hot button, as it has popped up again in a study that is current online at the Menopause journal site.
There are several conditions that affect work participation and demands, including menopause. And although there is some indication that abseenteeism is highest among women 45 years and older compared to their male contemporaries, the reasons have not been entirely elucidated. By gaining a better understanding of the factors that influence the balance between resources and work demands, there may be a greater openness to understanding and managing expectations by both the employee and the employer.
To explore this further, and using two scientific scales as a foundation, researchers looked into the severity and frequency of psychological, somatic, vasomotor and sexual symptoms and their potential impact on physical and mental work demands, health status and resources in208 women between the ages of 44 and 6o Additionally, they evaluated individual and lifestyle factors that might skew results, as it has been shown previously that among both men and women, lower education, older age, overweight, smoking and lack of exercise all negatively affected work ability.
The result? there was a negative and significant association between menopausal symptoms and work ability. Moreover, even after theyadjusted for some of the factors mentioned above, they found total work ability scores declined by almost a half a point for every one point on the total symptoms scale score. Mental health played a huge role as did somatic symptoms such as sleep disturbances, insomnia, joint pain or mood swings.
If these findings are extrapolated to real world situations, workplace interventions such as yoga breaks, exercise and stress reduction strategies, coupled with a self awareness of overall health and how symptoms detract from that (or not) are simple first steps towards finding a solution and improving work ability. The other piece of this, however, i.e. to openly communicate to our work colleagues, our managers, our partners and our friends how productivity and our relationships may be suffering and actively involve them in finding solutions, might not be so simple.
Often, one of first thing that’s pulled out of the aging hat is the fear that an employee is easily replaced. This has never been truer than in today’s economic environment where the numbers of willing and able workers are stacked against those who are holding onto their jobs by a string and a prayer. As a menopausal woman, do you really want to hand your employer a reason to replace you? I’m betting that the answer is no. Consequently, I am unclear about the best strategy for finding the elusive balance between work ability, resources and symptoms.
Any thoughts or ideas? I’d love to hear them. Let’s get a dialogue going, particularly if you are working harder for the money because of symptoms.
Read MoreWednesday Bubble: Timeout
Back in 2009 I posted a story about a woman’s death being blamed on menopause. It seems especially poignant a day after World Menopause Day, a day unlike any others, when we put down our prejudices and celebrate everything menopause.
As my grandmother would say “oy vey.”
How about we focus on how, as women, we are constantly manipulated by ‘disinterested’ parties? How about we call “timeout?”
A bit of context…
In 2009, the BBC ran a story about a woman who committed suicide. The headline read:
“Woman’s Death Blamed on Menopause.”
“A woman who refused to take hormone replacement therapy died while suffering a menopausal episode, an inquest had heard. Margaret Drew…was killed when she walked out of her family home on to a nearby railway line and was hit by a train…There is no trigger to this at all, except hormones making her do things that she normally wouldn’t do, Dr. Carlyon [Cornwall Coroner) concluded…”
Menopause. The silent killer. Oh really? Drew’s husband claims that his wife was “delightful, lovely and friendly” 99% of the time; the other 1% she’d become “totally irrational.” Yet, she refused to try HRT, he says. On the day of her suicide, he said that his wife was “clearly angry about something.”
Something.
Obviously, the conclusion is that that the “something” is hormones. This reminds me of vintage advertising copy that conveys the simple message that a pill a day can cure all that ails, wipe away the tears, mood swings and instability so that women can “transition without tears” (or better yet, without killing themselves).
Notably, a search in the National Library of Medicine’s PubMed database turned up only one recent study specifically dealing with suicide ideation across reproductive stages. In it, researchers compared data in 8,794 women, and found an increased risk of thinking about suicide among women during perimenopause, not before or after entering menopause. These findings remained after controlling for risk factors such as anxiety and mood disorders. HOWEVER, the researchers noted that the study design did not allow them to form any definitive conclusions about the specific reasons for thinking about suicide.
Another search yielded information that the risk for a major depression increases during perimenopause, primarily as the direct result of vasomotor symptoms. The same does not hold true for women before menopause begins or once they enter menopause. Note that while major depression is a risk factor for suicide, not everyone who is depressed will actually kill themselves.
Are hormonal fluctuations the sole cause of such deep unhappiness that women want to kill themselves? Or their careers?
Let’s look at a more recent story that appeared this week in the Denver Post.
“Former Elbert County assessor blames menopause medications for crimes, is sentenced to 60 days in jail, fined $10,000”
“Elbert County Judge Jeffrey Holmes might have thrown the book at former county assessor P.J. Trostel just for her management skills alone. Instead, he sentenced Trostel today to 60 days in county jail, three years of probation and 200 hours of community service on two felony counts…In asking for leniency, Trostel and her lawyer said a variety of factors led her to make bad decisions. Those included depression, symptoms from menopause, medications and stress from family and work. “Some of the things I don’t even have an answer,” Trostel said. “I know I made terrible judgments and decisions.”
It sounds as though Trostel would have done better with different legal representation. And a sounder argument.
And while Trostel is chewing on that concept for the next six years while incarcerated, perhaps we can start to change the paradigm and focus on the ills of the Menopause Industrial Complex, disinterested parties who perpetuate societal myths that menopause is a disease that requires treatment and that as women, our attitudes, belief systems and actions are hormonally-based and driven. That we are hysterical beings who need guidance on how to find our way and fulfill our dreams, realize our paths, but only if we calm down. That we can’t hold a job down, keep a marriage intact or play nicely with others. That we need a timeout (this would entail a long, long time, by the way).
Seriously though, a timeout from the hype would be a welcome addition to the change, don’t you think?
Read More
Needles and symptoms and a pathway, revealed…more on acupuncture
Click on acupuncture in the tag cloud and you’ll know that I’ve spent a number of years examining and sharing information about important studies on this blog. In some, acupuncture has been shown to alleviate vasomotor symptoms like hot flashes and night sweats, and in others, acupuncture appears to be no better than placebo or sham needles that are placed on accurate points but not actually inserted into the skin. However, I’ve also long argued that by slightly changing the way that we conduct scientific studies in the West and allowing for individualization, observed benefits might be different. Indeed, that’s exactly what researchers have seen with ACUFLASH and you can read more about that trial here.
Less clear that whether or not acupuncture can help symptoms (for the record, I am biased and I believe that over time it can), is HOW it works. The centuries old Chinese medicine paradigm is never so apparent than with acupuncture and although I am not sure why we need to know the ‘how,’ I am fairly certain that until it is revealed, there will be a lot of researchers and health practitioners questioning its validity or utility.
So, this brings me to a wonderful pilot study in the online version of Menopause, exploring that very question: how does acupuncture work on vasomotor symptoms?
In this small trial, 33 perimenopausal and postmenopausal received traditional acupuncture, sham acupuncture or nothing over a period of 12 weeks. The active groups received three treatments per week and all the women reported having at least 7 hot flashes a day. But there’s the rub: the researchers also looked at how traditional acupuncture affected the hypothalamic-pituitary axis (HPA), the part of the body that comprises the hypothalamus and pituitary and adrenal glands, controls digestion, our immune system, mood and emotions, sexuality, and how energy is used and stored. Moreover, this part of the body reacts quite negatively to stress by releasing a hormone known as cortisol. Not surprisingly, women who have very severe vasomotor symptoms tend to produce high levels of cortisol.
What did they learn?
- Most of the benefits, (e.g. reductions in hot flashes) occurred by week five and; hot flash severity and frequency declined by 86% and 78%, respectively in both the real acupuncture and sham acupuncture groups. But while the sham acupuncture group didn’t continue to improve, the real acupuncture group did.
- Likewise, anxiety and depression improved in both of these groups, as did sleep scores.
And the “how?”
It appears, at least from this small study, that acupuncture positively affected levels of cortisol and DHEA, the major steroid secreted by the adrenal glands that affects none other than the body’s production of estrogen. Consequently, if acupuncture helps to control the HPA, and HPA affects vasomotor symptoms, then perhaps scientists have the first clue as to why acupuncture may help certain menopausal symptoms. It also opens up an entirely new avenue for novel strategies to control them.
The bottom line is that there is hope and a new direction that researchers will ideally follow. Ultimately, acupuncture may prove to be even more effective than pharmaceutical strategies for menopausal symptoms and definitely, much safer.
The jury’s still out but it seems a helluva closer to a verdict.
Read More
Wednesday Bubble: Warn me
This week’s Bubble is straight out of the buyer beware files. Introducing Warmi ‘Better Menopause Relief.’
Warmi, according to the manufacturer website, is “a unique vegetable and fruit extract supplement. It contains 85% organic ingredients in a vegetable capsule and is 100% Vegetarian.” Moreover, Warmi provides safe, natural, full spectrum menopause relief” meaning that in a single study of 122 women, Warmi “also enhanced hormonal balance, mood, cardiovascular and bone health, vaginal dryness and intercourse discomfort — even overall quality of life. Many benefits were noted in just 30 days.”
Evidently, Warmi delivers, all that and more.
How, you ask?
Warmi’s active ingredients are:
- Gluocosinates, plant chemicals that are found in cruciferous vegetables such as cabbage, which are believed to help fight cancer and possibly, promote heart health.
- Beta-sitosterol, a substance found in plants and suggested to have properties similar to cholesterol. It is used in some European countries for benign prostatic hyperplasia (enlarged prostate) and according to the Warmi website, has been shown in laboratory animals to have some sort of weak estrogen effect that “may benefit the reproductive system.”
- Hesperidin, a flavonoid found in citrus fruits which has shown promise in laboratory animals to potentially reduce blood pressure and cholesterol and work as an anti inflammatory and produce pain killing effects. The Warmi website says that it may also ‘help bone metabolism.’ Note that this claim is based on one study done in mice, which demonstrated a decline in the loss of bone density.
So, Warmi is made up of cancer and heart protective ingredients, may alleviate pain, and…helps with menopausal symptoms? But how does it work? In the FAQ section of the product website, it says that while “The exact mechanism of Warmi is not fully understood but is believed to be associated with certain estrogen receptors.”
I’m sorry…WHAT?!
All I can think of when I think ‘Warmi’ is “warn me.” Yes, warn me that medical and scientific claims without substantiation are to be questioned, that comparisons to existing alternative strategies are difficult without well-designed research, and that unpublished, unreviewed product data are just that: unpublished, unreviewed and non-vetted.
Forewarned is forearmed.
Enough said.
Read More
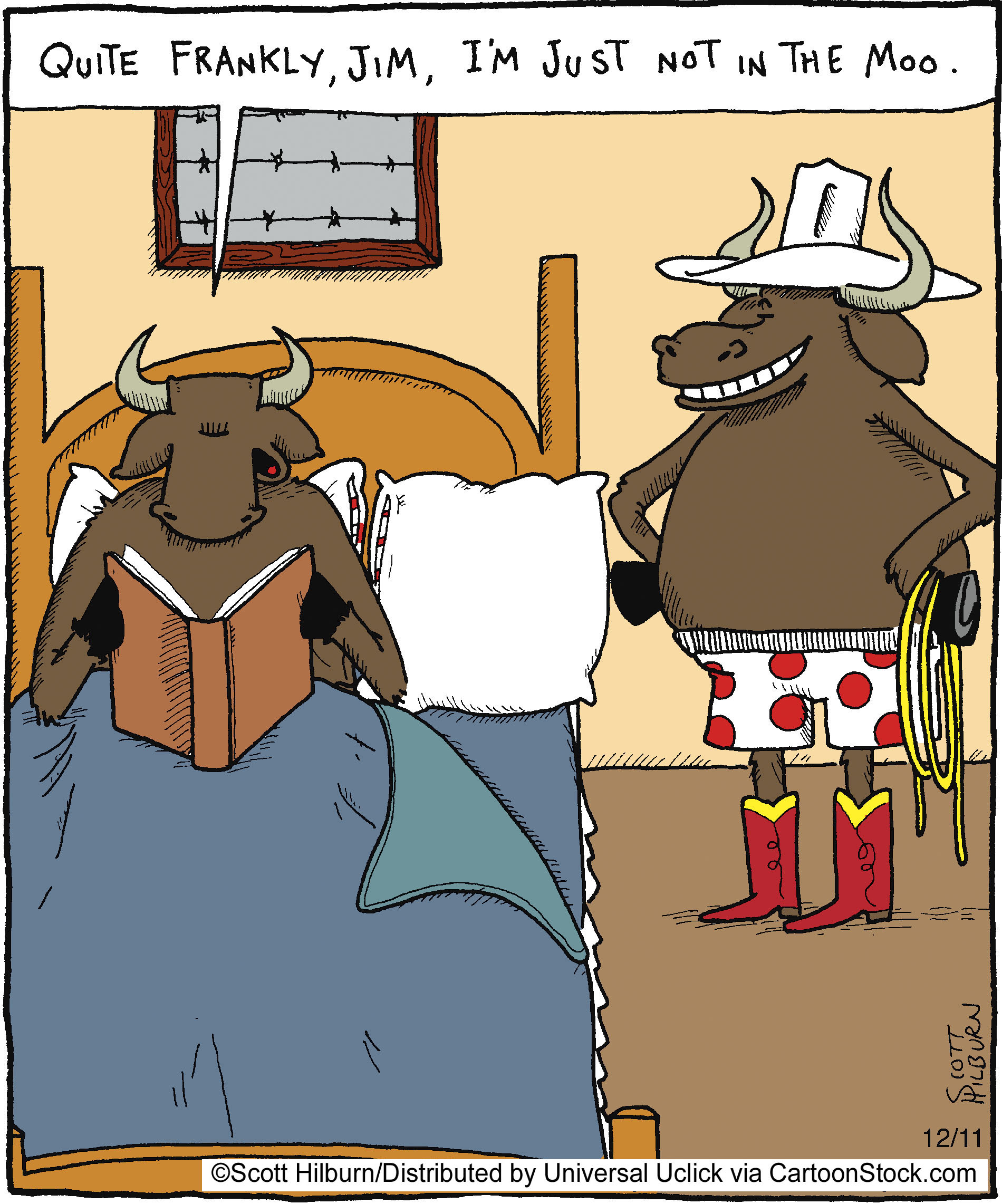
Wednesday Bubble: Are you in the moo? Sex and a sense of purpose
What are we bursting this week? How about midlife and sexual desire. Frankly, I’ve got sex on the brain, sex in midlife, that is. And what we need to do to insure that it continues to be enjoyable, that we desire it and that we please our partners as much as we hope that they please us. Consequently, I am reposting this piece from earlier in the year, with the hope that with a sense of purpose, you’ll become more in the moo. Or mood. Whatever the case may be.
Sexual desire. In midlife, sexual function and sexual desire aren’t well understood, primarily because there are so many factors that enter into equation. This may be why certain silver bullets, like a female viagra, has failed to show any significant improvements in the desire department. And yet, researchers continue to accrue more information about the things that influence desire in women, ranging from the quality of intimate relationships to social support and overall wellbeing. The manufacturer who discovers a pill that addresses all of these will have struck gold. Meanwhile, back in reality, as many as 75% of women in midlife rate sexual health as important enough to warrant further exploration.
Fortunately, we may have another piece of the puzzle: ‘sense of purpose,’ which appears to be associated with greater wellbeing, happiness, life satisfaction, self-esteem, personal growth and optimism. A sense of purpose also appears to improve health, prevent certain diseases and may even improve cognitive function, thereby staving off mental diseases associated with aging. In a study that appears in the online version of Menopause, 459 menopausal women who were sexually active with a partner were followed over three years. Each year, they were asked about their emotional wellbeing (including their general mood, anxiety and depression as well as how often they engaged in and enjoyed sexual activity (specifically desire, type of activity and hugging and kissing). In the final year, they took a test that rated their sense of purpose on a five point scale ranging from ‘there is not enough purpose in my life’ to ‘the things I do are all worthwhile.’
The findings?
A greater sense of purpose equaled a great enjoyment of sexual activities, independent and regardless of other specific life circumstances. In other words, psychosocial functioning, e.g. social support, quality intimacy and overall wellbeing influenced the quality of these women’s sexual lives. On the other hand, menopausal status and use of hormone therapy did not appear to play a significant role in how often women engaged in sex or if they enjoyed it. This is important, as it means that psychosocial wellbeing may ultimately be more important than hormones.
In so far as the desire to engage? Women who were younger, had more social support, felt better about themselves and weren’t suffering from vaginal dryness tended to want sex more than their older peers who didn’t enjoy these factors.
Not surprisingly, many of the factors that researchers stress may help desire and engagement are associated with greater nitric oxide levels, which Dr. Christina Northrup says can help combat sexual dysfunction and improve pleasure.
When it comes to sex in midlife? It may help to think ‘sense of purpose,’ a real sense of purpose, now. (Poetic license, Chrissie!) I’m all for it if improves activity and desire without drugs.
Read MoreBreathe. What you need to know about asthma and HRT
If you suffer from asthma, you will want to take note: researchers presenting at this week’s European Respiratory Society AnnualConference have shown that female asthmatics have an increased risk of landing in the hospital if they take hormone replacement therapy (HRT). Yet another nail in the HRT coffin, once again demonstrating that the health risks of taking hormone replacement may outweigh the benefits.
Notably, studies have shown that asthma risk increases in women after puberty. Moreover, hormones, most specifically fluctuating estrogen levels, can impact airways as much as allergies and hay fever (fluctuating estrogen levels can produce an inflammatory response and exacerbate breathing difficulties). On average, asthma symptoms develop in about 21% of menopausal women and more than twice as many using hormone therapy.
In this study of over 23,000 Danish women with documented asthma, researchers looked specifically at hospitalizations for severe reactions. They also collected information on smoking, exposure to smoke, body mass index, level of physical activity, history of hysterectomy and use of HRT. The findings? Using HRT increased the risk for hospitalization for severe asthma reactions by as much as 40% compared to not using hormone therapy. What’s more, the longer the women used HRT, the higher their risk of ending up in the hospital; for example, if they used it for less than 3 years, they have a 29% increased risk and if they used it for more than 10, a 51% increased risk. Even more troubling was the fact that women didn’t smoke appeared to have the highest risk for being hospitalized in association with their HRT use.
Although this isn’t a randomized trial, and more information is needed, the researchers still recommend that practitioners be made aware of these findings. They say that the relationship between asthma and female sex hormones is hardly new, but that their findings confirm the relationship and further our understanding of it by showing the extent of severe asthma reactions that occur when women take hormones. “If a patient develops asthma or has a severe worsening of symptoms after taking HRT, they may need to stop hormone therapy altogether,” they add.
Read More