Wednesday Bubble: What did I forget/hear/see/say…
If you’re anything like me, you are starting to forget things. Things you need to do, why you walk into rooms, shopping lists, things you said, the whole nine yards. For me, it’s become the norm, not the exception and while I spend a lot of time making jokes about it, it also drives me crazy.
Yet, today’s Bubble is not one that I’m likely to forget. I’d like to think of it as one part inspiration and one part WTF? And it leaves me with a whole lot of questions to boot.
Study findings suggest that gaining weight during menopause may increase the risk for loss of gray matter. Gray matter refers to the cortex of the brain, which contains nerve cells. It is involved in muscle control, sensory perception (seeing/hearing), emotions, speech and finally, memory.
In this study, which was published in the online edition of the journal Psychosomatic Medicine, researchers evaluated brain imaging data, demographic information (height, weight) and behavioral measures (perceived psychiatric stress) obtained from 48 healthy postmenopausal women. Data were collected over a 20-year period.
The findings showed a unique association between increase in body weight during the transition from peri- to post-menopause (as measured by body mass index or BMI) and a 22% reduction in grey matter volume. These findings occurred in women who were otherwise healthy, had no history of heart disease or psychiatric illness and did not meet the threshold for obesity (>30 BMI). All women had also undergone natural menopause.
The researchers suggest that weight gain during menopause is a “highly modifiable risk factor” that may help to prevent or slow “potential alterations in brain function that are important to quality of life.”
I’ve written previous posts on cognitive issues during menopause, whether they be linked with life stressors, HRT or aging. Now it seems that researchers are telling us that weight gain may also be a risk factor.
Less clear is how much weight gain and what we should do about it. In general one solution to combating weight gain in midlife is restraint. Coupled with exercise, this may just be the magic formula. In the meantime, I think that we need a few more studies to take a closer look at brain matter changes in midlife.
What do you think?
I just forgot why I’m asking you that…!
Read MoreWednesday bubble: age ain’t nothing but a…

Number?
Sometimes it is just that. And sometimes it’s not.
Confused yet? I certainly am.
Australian researchers suggest that many of the more common complaints of menopause may be possibly related to aging in general and not specifically the transition. In fact, in a study presented during last month’s 8th European Congress on Menopause, they reported that menopause is strongly associated with some but not other common complaints.
So what about the other symptoms? After reviewing data from 58,724 women (ages 45 to 50) participating in the Australian Longitudinal Study on Women’s Health, the strongest associations were seen between menopause and hot flashes/night sweats. These findings remained after adjusting for age during the study, age at menopause, smoking history, body mass index, sociodemographics (i.e. education, income, marital status and geographic location) and other factors that might influence outcomes. Other symptoms, including difficulty sleeping, stiff/painful joints and poor or fair self-reported health were also associated with menopause but to a much lesser extent. Headaches, migraines and incontinence appeared to be more strongly related to the aging process.
The researchers say that treatment (in this case, HRT) should be geared primarily towards alleviating vasomotor symptoms. Less clear, however, is how long therapy should be continued, since some symptoms can last for more than seven years. This study is scheduled to appear in Menopause.
Last September, I wrote a post about a survey being reported at the North American Menopause Society’s Annual meeting suggesting that women can actually discern the symptoms of menopause from those of aging. Interestingly, many of the symptoms overlapped; in fact, 84%, 72%, and 77% of respondents associated vaginal dryness, urinary stress incontinence and weight gain, respectively, strictly with menopause, even though they can also be caused by aging as well.
So, what’s the primary point? It can be difficult to tease apart the effects of aging and the effects of menopause. Clearly, these new Australian data add a bit more to the confusion, and reinforce the point that more research and funding is needed in this particular area.
In the interim, I am just as happy to blame the ‘pause for my symptoms as I am to blame age. And equally as happy to take positive steps to overcome some of the more troublesome effects of the transition, regardless of whether it is a direct effect of menopause or not.
All in all, a good thing, right?
Read MoreShe’s so hot…and it’s so cold

I ran across a wonderful review and commentary on Louise Foxcroft’s ‘Hot Flushes, Cold Science’ in the Lancet journal this past weekend.
Writer Londa Schiebinger points out the Foxcroft details how western medicine took “a natural process” and made it into a disease. [The book] “tells a much needed story — it’s a must read for those who don’t know how western medicine has created dread and shame in menopausal women. Foxcroft reveals the underbelly of a history [of physician’s attitudes towards and treatments of menopause] rife with chauvinism, misogyny and collusion. It also reminds us of the need for good medical research in this area.”
Some of the more drastic treatments throughout the 19th through 21st Centuries have included:
- Removal of one or both of the ovaries (which was associated with a death rate of 45%)
- Radiating ovaries to restore femininity
- HRT and its associated cancer and heart disease risks
All of these, being sold to millions of women, of course, on the premise that menopause is truly a woman’s hell.
Even though the National Institutes of Health has specifically stated that menopause is not a disease, many western practitioners continue to perpetuate the myth and line the pockets of the pharmaceutical companies. However, Schiebinger reminds us that “women’s power, including the power to say “no,” may be their best defense against the maladies” that our culture associates with menopause.
I am inspired by the upsurge in interest and research into alternative approaches to address menopausal symptoms, by the strength that many women are now showing by refusing to start hormone therapy or insisting that they wean off of it, by writers like Foxcroft who are ballsy enough to confront the status quo and insist that women be encouraged to take control over their healthcare and their bodies.
I started Flashfree a little over a year ago with a mission to provide timely information about alternative approaches to menopause and to encourage women to create a new paradigm about midlife and its challenges. Undoubtedly, science has its place in helping us toward some of these goals. However, only by constantly challenging and pushing back will we be able to truly become masters over our own destinies.
Read MoreWednesday Bubble: something for da guyz

Men! Male menopause? I think not! The closest thing to it? I believe so.
New York Times writer Dana Jennings, wrote a poignant piece in yesterday’s paper about his personal experience with hot flashes — not only as a husband/partner to a menopausal woman — but also as an advanced prostate cancer patient taking Lupron for his condition. Entitled “My Brief Life as a Woman,” (a title, which by the way, I want to rebel against) Jennings explores the effect that hormone therapy had on his body (night sweats, weight gain), his emotions (fits of crying), energy (fatigue) and overall quality of life (frequent headaches).
What resonates? His admission that “even though I only got to spend a brief time on the outer precincts of menopause, it did confirm my lifelong sense that the world of women is hormonal and mysterious, and that we men don’t have the semblance of a clue.”
I applaud Jennings for his candor, his sensitivity and his humour.
Men – the next time your wife/partner/girlfriend/friend is on the “Good Ship Menopause,” as Jennings so aptly describes it, embrace and offer to carry her “physical baggage.” Although it’s not a trip you’re necessarily prepared for, the journey may help you understand what she is going through a bit more thoroughly. Another helpful resource: Dick Roth’s “No, It’s Not Hot in Here,” a husband’s guide to understanding menopause.
A little understanding, a little support, and someone to sit with during bad chick flicks. Is that too much to ask?!
(Thanks to Steve Woodruff for pointing me to this piece in the NYT)
Read MoreMore joys of soy
More news on soy. Researchers have discovered yet another component of soy isoflavones that may prove useful in improving symptoms of menopause: soy aglycons of isoflavones (SAI). Soy aglycons are a group of chemicals found in fermented soybeans and comprise a great portion of diets for Chinese and Japanese individuals. Of note, high cholesterol, coronary heart disease, and menopausal symptoms are often seen in a smaller percentage of these women than their European and American counterparts.
Among the various chemical molecules of soy, SAI are absorbed faster and more efficiently than other components.
In this particular study, which was just published in Nutrition & Metabolism, researchers fed rats whose ovaries had been removed either high or low doses of SAI-supplemented diets. These animals were then compared to rats with intact ovaries who were fed a regular diet.
The researchers found that rats fed supplemental SAI had significantly lower cholesterol and low-density lipoprotein (LDL) values , higher high-density lipoprotein (HDL) levels and faster liver metabolism. The lining of the uterus was also enhanced by dietary SAI supplementation.
They said that these results suggest that SAI may help protect against or lessen symptoms during menopause that are associated with the natural decline of estrogen. SAI might also be an effective and safe alternative to HRT, which has been linked to breast and uterine cancers. In general, SAI may protect against menopausal heart disease.
Read MoreTick, tock…
I ran across an interesting study the other day that suggests that a simple blood test can predict when women will enter menopause.
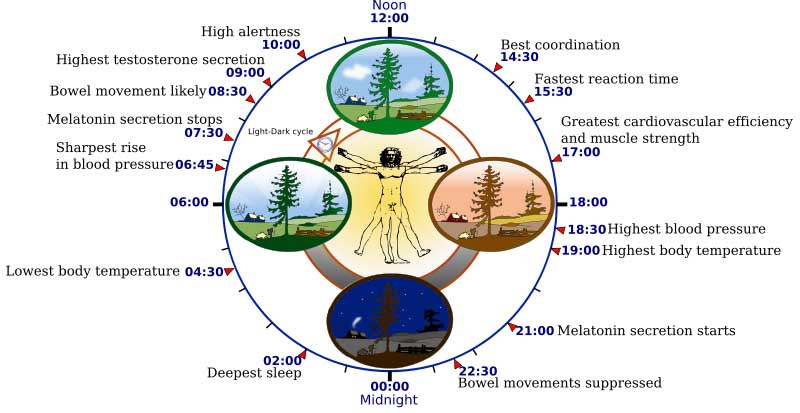
Although the test is used primarily in the fertility setting (to measure the size of the ovarian follicle pool, if you will), it got me thinking: could it be useful during pre-menopause to predict timing and allow for ample time to, say, engage in more healthy bone-building or heart-strengthening habits or start developing mind-body strategies that reduce stress and promote the production of nitric oxide? Better yet, is this blood test a tool or marker of time that a major life transition is upon us and prompt us to pay attention to ourselves and start doing things that not only benefit our loved ones but also ourselves?
Reporting in the Journal of Clinical Endocrinology last year, researchers said that they have developed a blood test that measures a hormone known as “anti-Mullerian hormone” (AMH). AMH correlates to immature follicles in the ovaries whose role it is to house mature eggs. The greater the number of these follicles, the more likely it is that a woman will conceive.
In the study, AMH levels were measured in 144 fertile women between the ages of 26 and 46. Researchers then set a baseline level and compared them to the AMH levels in women who had undergone menopause. They were then able to observe that there was a close correlation between declining AMH levels and the age that which menopause began.
Although additional studies are clearly needed to support these findings, some infertility clinics are evidently already using AMH as a marker for a patient’s fertility “potential.” According to an article on the study that appeared in Time magazine last year, the blood test might also be useful in cancer patients to measure the impact of chemotherapy on fertility.
In the interim, it is interesting to consider the utility of the AMH blood test for women in midlife so that they can take steps to insure wellbeing and optimal health during the menopause.
Food for thought.
Read More





