Sex on the beach

Okay. I’m not really going to write about having sex on a beach or that tropical drink. But now that I have your attention, I want to bring attention to a new study that I stumbled across recently.
This particular topic is of interest to me and clearly, I’ve written about sex and the transition numerous times. And since I’m in the middle of Dr. Christine Northrup’s ‘The Secret Pleasures of Menopause’ I do have sex on the brain at the moment. More on the book at a later date.
Although sexual concerns are reportedly very common among menopausal women, low sexual function can be attributed to many factors, including attitudes and beliefs about the transition, changes in body image, health, stress, fatigue, partner’s sexual function, and the role of intimacy in the relationship. Importantly, up to 47% of women may experience depression during menopause and in fact, findings from the Massachusetts Women’s Health Study suggest that aging and menopause affect sexual function less than general and mental health.
In this particular study, published in the online edition of the journal Maturitas, Turkish researchers evaluated association between depression and change in sexual function in 300 women in menopause.
Among the participants, 65% had low sexual function. This included low desire (40%), low arousal (82.7%), low lubrication (63%), low orgasm (75%), low satisfaction (82.7%), and pain during sexual activity (54.3%).
Although only a third (29.3%) of women were identified as having depression, the researchers found a significant association between desire and depression scores throughout the menopausal transition. As depression increased, so did sexual dysfunction.
These findings imply that sexual dysfunction during menoapuse may be as much a result of atttitude and emotional health as hormones if not more so.
Dr. Christine Northrup explores some interesting solution to these problems. Stay tuned!
Read MoreMore Sex: Another One Bites the Dust
[youtube=http://www.youtube.com/watch?v=hMenB9Ywh2Q]
Guess that I have sex on the brain these days.
Another theoretical benefit of HRT bites the dust. Researchers at McGill University’s Laboratory for the Biopsychosocial Study of Sexuality have found that HRT is ineffective for alleviating painful sexual intercourse in a majority of postmenopausal women.
Approximately one in three postmenopausal women suffer from dyspareunia, or pain during intercourse. This has historically been attributed to declining estrogen levels and changes in the genital tract that lead to thinning skin. HRT has long been used to treat this problem.
The McGill research team, led by Alina Kao, say that their findings suggest that numerous conditions that may be causing pain, such as infections or problems with pelvic floor muscles, are apparently being overlooked by most clinicians. Consequently, they suggest that treatment should be individualized.
The study is slated for publication in the journal Pain Research and Management. In the interim, you can learn more about the lab’s work here.
Read MoreLibido
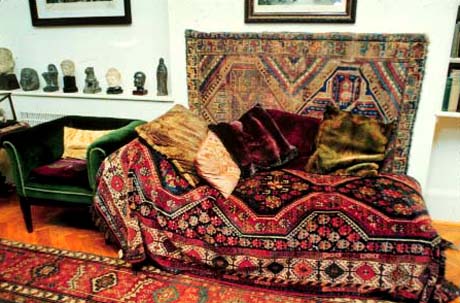
Many clients of Sigmund Freud spent hours on his infamous couch (pictured) discussing their libido (or lack thereof). Freud invented the term to describe sexual drive in his patients, and believed that sexual experiences in infancy were what drove later emotional issues in adulthood.
Other psychologists (e.g., Carl Jung) have debunked Freud’s theories and more contemporary experts in the field believe that while libido is rooted in hormones, it is largely driven by culture and individual experience.
Here’s a stat:
Approximately 70% of post-menopausal women experience a loss of libido.
Undoubtedly, declining hormones play a large role in loss of sexual interest and desire after menopause. But have you considered how emotions and self-esteem may come into play as well?
So far as I am concerned, there is no reason why women can’t enjoy a healthy and exciting sex life during and after menopause. In fact, although hormones like androgens may influence libido or behavior, they reportedly have less of an impact on the ability to reach orgasm. This suggests that perhaps, how we feel about ourselves during this transition, coupled with the societal stigma of aging, may play a role in our sexuality.
So, how do we change this perception?
Sex expert Betty Dodson spiced up her postmenopausal life by playing a call girl. Okay, that’s a bit extreme for most of us but it certainly gives a new meaning to role play. For the rest of us, regaining one’s sex life during and after the transition may require a new approach, new tools and some creativity.
Any thoughts? Email me privately and I’ll summarize in an upcoming post.
Read MoreLet’s talk about sex
[youtube=http://youtube.com/watch?v=qzfo4txaQJA]
I’ve heard that menopause is often linked to problems in sexual functioning.
Now mind you, this is one issue that many of my gal pals, present company included, have yet to experience but I believe that it’s an important topic nevertheless. Indeed, other women have expressed issues around desire, capacity for orgasm, and frequency of intercourse. The question is, are these problems related to menopause and hormones or to aging? Well, apparently both.
For example, some studies have found that the sharpest decline in sexual interest for women occurs around the mean age of menopause, while others have found that menopausal status (i.e., the point of the transition) negatively affects sexual function independent of age.
Interestingly, one of the largest studies – the Melbourne Women’s Midlife Health Project – which followed 438 women through menopause for more than 10 years, found significant declines in female sexual functioning, responsiveness, frequency of sexual activity and libido. When the researchers compared women who went through the transition during the study to those who remained pretty much in the same phase, they found that only sexual responsiveness declined. What this implies is that our ability to respond to sexual activity is paired with aging, while all the rest of the issues, are affected by menopause.
Interestingly, among the variety of factors that may contribute (e.g. quality of intimate relationship, degree of stress, general well-being) androgen levels (i.e., testosterone) may play a role.
In a fairly recent review of 14 controlled trials in women undergoing natural or surgical menopause, researchers found a benefit from “adding back” testosterone, in terms of sexual desire, frequency, pleasure, and satisfaction. Testosterone was administered via patch, a gel, and inhaled, among others. While some of the benefits may be attributed to the so-called “placebo effect,” the results are interesting and lend promise for future studies.
Read More





