I’m so dizzy…
my head is spinning.
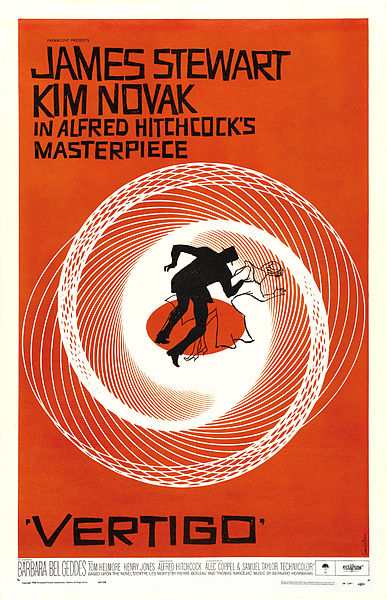
Those of you in my generation will remember this song by Vic Reeves with the Wonder Stuff. Talk about a one hit wonder! Or Vertigo, the incredible film by Alfred Hitchcock. But, dizziness is anything but wondrous and having suffered a form of vertigo that occurs when the head changes position (also known as benign paroxysmal positional vertigo or BPPV)), I can share that it’s an awful experience. The last time it happened, I didn’t leave the house, didn’t drive and required motion sickness pills to sleep.
The reason why I’m sharing this with you is that BPPV occurs in at least twice as many women as men and its likelihood increases with aging. More troubling is the fact that study findings suggest that hormonal fluctuations — especially during menopause — appear to play a role. Historically, BPPV has been linked to the dislodging of crystals in the inner ear, which causes a greater sensitivity to gravity. Thereafter, changes in head position, for example, lying down, looking up or turning over in bed can cause brief vertigo spells. Although most of the time researchers don’t know why it occurs in some people versus others, BPPV has been linked to head trauma other ear conditions.
The most current research comes from a study of over 1,300 individuals, almost 1,000 of whom were women. I’ve already noted that in the general population, BPPV occurs in twice as many women as men. In this population, not only were women in the 40s three times as likely as their male peers to develop BPPV, but most of them reported being in perimenopause, suggesting that hormonal fluctuations , especially estrogen, were at play. What’s more, some data suggest that there is as we age, there is a deterioration in the protein that help anchor the inner ear crystals, and estrogen appears to help promote this.
The silver lining is that while there is little that can be done about aging and estrogen’s role in BPPV, the problem can be successfully addressed with a series of head maneuvers that help restore the crystals back to their former position. Still, I personally find that I get periodic vertigo sensations at the oddest times and that they tend to worsen during my worst hormone movements.
Dizzy Lizzie? Sure, I’ll admit to it. What about you?
Read MoreDeath be not complacent
 Pete Seeger died last week. He was 94. As a lover of folk music, it’s hard to imagine someone who more powerfully embodied that genre’s ideals. A man of principle who believed the best thing to do with a song was share it, a man who used his music like a well from which to draw joy.
Pete Seeger died last week. He was 94. As a lover of folk music, it’s hard to imagine someone who more powerfully embodied that genre’s ideals. A man of principle who believed the best thing to do with a song was share it, a man who used his music like a well from which to draw joy.
What struck me as I read the many tributes to him in emails, tweets, and Facebook posts was that death is different as you age. I lost an older brother at 13. That was a shattering experience. In my 20s, I can only remember going to one funeral – a young man who died tragically in a roller-blading accident. It was a poignant service.
By now, I’ve lost tons of uncles and aunts from my long-lived clan; too many. The most recent was just last week, my aunt Stella. A few cousins too, and of course, my dad. And outside of the family, I’ve lost friends, primarily to cancer, that blind killer of the old and young alike.
I have had more encounters with death than I’d prefer. But what once was momentous has become an event that is sad, inevitable, and far more anticipated than before. So what should we men of a certain age learn from death?
Don’t sit on things. When I was diagnosed with bladder cancer, it was caught early because when I saw blood in my urine, I DID something about it. Ignoring symptoms is rarely a good idea.
Acknowledge your own mortality. Yes, you feel good now. It’s easy to tell yourself — seriously — that you’re bulletproof. But be realistic. Bodies change, fitness changes; if you are an average guy, you’re likely not as strong as you were 20 years ago, as fast. Accept it (without giving in and giving up). Set fitness and activity goals that aren’t going to leave you groaning for days afterward or in the ER.
Do stuff now. When I turned 40 and got cancer, it woke me up and I made some changes that I’d idly thought and talked about for years without taking action. It’s always time to do that. Investment guru John Templeton once said “The best time to invest is when you have money. This is because history suggests it is not timing the markets that matters, it is time.” You HAVE time that you can invest in anything you want to do. Right now. Do something.
Think a little bit holistically. No, I’m not suggesting buying a juicer or getting your chakras aligned. But when I was younger, I didn’t make the connection between my body and my mind. Using tools like yoga, meditation, therapy, etc. doesn’t only improve your psychological health. It can make you exercise better and, in my experience, make you enjoy your exercise routine more by deepening your concentration.
Death is inevitable. It’s going to come to all of us at some point, and we will be reminded of that by the loss of friends and family from time to time. But don’t take that inevitability as impending doom; take it as a reminder that with a finite amount of time allocated, it’s up to us to make the most of it.
(photo Creative Commons licenced by Flickr user Leiris202)
Read MoreNewsflash: Yoga and hot flashes
When it comes to alternative strategies for managing hot flashes, where do you turn? I’ve been writing about alternatives for five years now and the only thing I am fairly certain of is that what works for one woman doesn’t necessarily work for the next. Consider the management of menopausal symptoms similar to the management of any condition: the best treatment is always individualized.
Still, mind-body practices tend to rise to fore and evidence continues to accumulate supporting their value and usefulness. This is especially true of meditation, and of yoga.
The latest news on yoga comes from the online edition of Menopause journal and researchers are saying that integral yoga practice may help to reduce hot flash frequency among some women.
Integral yoga integrates the various branches of yoga and focuses on a whole body approach with the goal of transforming the entire being. Experts say that it is especially well suited to hot flashes because it emphasizes stress reduction and decreasing the likelihood of becoming overheated.
To evaluate its usefulness in a more scientific setting, researchers asked a small group of women in perimenopause who reported at least four hot flashes a day to participate in 10 weekly, 90-minutes integral yoga classes comprising breathing, centering medication, physical postures and deep relaxation, or health and wellness classes on different topics relevant to menopause and midlife women’s health or no interventions at all. All had the option to join classes at any time, and were required to fill out diaries about their flashes.
The findings? The researchers say that even after controlling for a potential placebo effect, both the yoga and health and wellness groups tended to follow a similar pattern and a similar significant decline in hot flash frequency. Women in these groups reported an estimated 66% (yoga) and 63% (health/wellness) decrease in the frequency of their hot flashes. And, while the effectiveness of yoga to lower hot flash frequency was not considerably different than that of the health/wellness education classes, the inclusion of the two behavioral interventions may perhaps capture naysayers’ attention; most studies only include on behavioral intervention and having two helps to temper bias.
We need more studies like this one to tease out the benefits of behavioral interventions. The good news is that the information is there for those who look deeply enough.
Read MoreStill flashing after all these years…
 Oy! I’ve got some rather troubling news to share: your hot flashes may continue for up to 9 years after menopause begins and in some women, they may continue past the 10 year point.
Oy! I’ve got some rather troubling news to share: your hot flashes may continue for up to 9 years after menopause begins and in some women, they may continue past the 10 year point.
Findings from the Penn Ovarian Study suggest that in women with moderate to severe hot flashes, almost half will see their flashes peak during the two years after menstruation stops and then they will continue to decline slowly to premeonpausal levels. Overall, in the 255 women studied, hot flashes lasted a mean 4.6 years among all women regardless of severity, while women with the worst symptoms had hot flashes that lasted nearly two times longer than their peers.
In this group of women, important factors influencing hot flashes included FSH levels before the final menstrual period, body mass index, and anxiety. And, not surprisingly, when the total duration of hot flashes was considered, including the time in perimenopause, African-American women had longer mean total duration of hot flashes (9.5 years) compared to white women. Previous studies have also shown that race is a factor when it comes to menopausal symptom severity and duration.
The study lasted 16 years and the researchers say that it’s not clear how the numbers would have changed had the women been studied longer. Additionally, current hormone users and women who went into early menopause due to surgery were not included, meaning that the findings might not be generalizable to a pool of women beyond healthy African-American and white women with untreated symptoms.
Still, the findings show that women can expect their hot flashes to last an average of four to five years after their final menstrual period. This emphasizes the importance of preparation and establishing a relationship with a knowledgeable health practitioner so that regimens and strategies can be modified accordingly throughout the pause… The more you know!
Read More
Guyside: Who says prevention is worse than the cure?!
Hey Guyz…
My partner in crime, Bob LeDrew is off paving his own preventive highway. He’ll be back next week with another edition of Guyside. Meanwhile?
Just a thought to ponder on a Wednesday….
Read More
Empowering Myself Before & After Surgery: Guest Post by Cyma Shapiro
Did you catch last Friday’s post about reaching deep to find the strength to ask for help? Cyma Shapiro, author of The Zen of Midlife Mothering, did and sent me a wonderful post about her own surgical experience in solidarity. Here it is, in its entirety; I hope that it inspires you as much as it did me.
I’ve been very lucky. In my lifetime, I’ve enjoyed good health, good friends and not a lot of unforeseen external circumstances. However, this recently changed when I needed surgery.
It’s difficult to explain the (many) steps I took leading up to this decision, but as insignificant as it might have been, how monumental it all felt. And, while there are far more people struggling with far more serious illnesses, my recent foot surgery was so pivotal in my life that I’d like to share my short journey with you.
As an avid and passionate proponent of Eastern modalities, I’ve spent an entire lifetime focusing on healthy eating, healthy living and healthy practices. I believed that in doing all of this, I’d be spared more serious complications. So, when I broke my foot last year, I felt as if my world had shattered. I was literally stopped dead in my tracks – a difficult journey for someone as active as I am (rock climb, bike, hike, etc.). I had no choice but to heed the call. And, I needed to do just what the doctor ordered: stop.
So, for six months, I tried to smell the roses: I reflected on the state of my life and of my “mid-age.” I thought long and hard about the things that I did and didn’t accomplish, and of the….well….mortality of it all. Most importantly, I realized that my apparently well-ordered life was certainly not that – that many more things (than I’d ever considered or thought possible) were simply out of my control.
To me, having surgery felt like death – not only for the potential perils and outcome, but for what the circumstances suggested – that I simply was no longer as immortal as I believed.
And so, in counting down the months, then weeks, and then days before the surgery, I fervently kept up every practice I knew – praying, breathing, exercising, meditating, reading, etc. And, as the weeks became days, I nearly lay myself prostrate in asking for help, guidance and support during this period. I also did one more thing: I asked my closest friends to pray for me and send light and love.
Nearly immediately, I felt an energy shift in my body. And, as much as the panic threatened to overtake me, the internal support I felt helped propel me forward.
On the day of surgery, I asked for help from the support nurses (requesting that they hold my hand and pray for me) and told the doctor that I had prayed for him. (I had, asking for guidance and love from the support team. To me, we were all in this together – I’d put a photo of him up on my computer weeks earlier.)
Today, I am healing. I am also doing fine. However, I have also changed – in my feelings about Western medicine, about how a higher power is truly in charge, in learning how tough and resilient I really am (despite my overwhelming fears otherwise), and how the power of others can support you in your life.
While I realize that some of you may scoff at this, believing this to be a minor blip in the journey of life, I believe that the success I’ve experienced here will translate into greater successes, should more serious things arise in my life. And, for this deeper understanding and in climbing another rung of life’s many twists and turns, I am so very grateful.
About Cyma…
Cyma Shapiro, 56, is the writer/creator of NURTURE: Stories of New Midlife Mothers (www.MidlifeMothers.org), the first art gallery show dedicated to women choosing motherhood over 40 (now traveling North America), and the subsequent blogsite, www.MotheringintheMiddle.com, for all-things midlife mothers. A speaker and writer for several sites including Huffington Post, whose work has been featured on NPR and on Psychology Today (online), Cyma is passionate about supporting women who choose later motherhood, and giving them a face, voice, and forum. She is the mother of 9 and 11-year-old children and 28 and 30-year-old stepchildren. She recently published The Zen of Midlife Mothering (essays from MotheringintheMiddle.com) – the only anthology on the market by and for midlife mothers (and fathers).
Read More
Help!
If you are as independent as I am, asking for help might be alien to you. Personally, I am getting better at it. But I still have the inclination to try to do something first on my own rather than rely on someone else to do for me, even if it may be detrimental.
I am having surgery today. I’ve been in significant discomfort for weeks now and that discomfort has been increasing daily. And I was going to drive myself to the procedure until my friends stepped in and took over. Don’t you think that I would realize how silly that idea was?
So, while I spend today contemplating the ‘thank goodness, folks who love me stepped in,” I challenge you to ask yourselves the following question:
When was the last time you asked for help? Better yet, how easily do you ask for and receive help?
Reading Karen Rosenthal Hilsberg’s “Lessons in Living” and her struggle to make sense of a life unraveled as her husband dies, I can’t help but reflect on a close friend who was ill several years ago. Despite a ‘take no prisoners’ attitude, he had trouble acknowledging the seriousness of his condition and even more trouble asking for support. Quite honestly, he doesn’t do too well in that department and neither do I. However, like him, I readily offer assistance to those I love and care about, whenever I can.
So, why the divide between offering and taking?
Hilsberg writes that “what I learned during this intense time of life was profound. I learned to ask for help from others.” Utilizing the mindfulness practice of the Zen Master, Buddhist monk and scholar Thich Nhat Hanh and the Buddhist Master Thich Phuoc Tinh, she says that she discovered that asking for help really wasn’t much different than providing it, that the helper and ‘helpee’ were intertwined, unable to exist without the other. By allowing assistance, she was able to provide others who cared about her and her family an opportunity to “be of service and to practice generosity” and in doing so, make a shift away trying to do everything on her own. Most importantly, by reflecting on how much she personally enjoyed being of service when loved ones needed her, she was able to accept how appropriate and okay it was to actually ask for help from others — to allow them to “do” as much as she did. The result? Her “wellbeing improved as [she] felt [her] burden shared by many hands.”
As caretakers, many women often do not adapt well to being on the “receiving end.” And yet, most of us are aware of the importance of social ties, friendships and support to our health and wellbeing, particularly as we age. So why do we find it so difficult to ask for and receive help? How do we acknowledge that be cared for does not equate to losing power or control but actually improves outlook, wellbeing, and ability to deal with any challenges that we might be facing, that allowing others to “do” empowers and does not ‘de-power?’ Is it fear of refusal? Or fear of letting go?
Mastering the art of asking for help is difficult. However, it behooves us to do so, not only for our wellbeing but for the wellbeing of those around us who wish to help.
My friend deserved the kind of care that he has provided to others in his life for most of his life.
Guess what?
So do I.
And so do you.