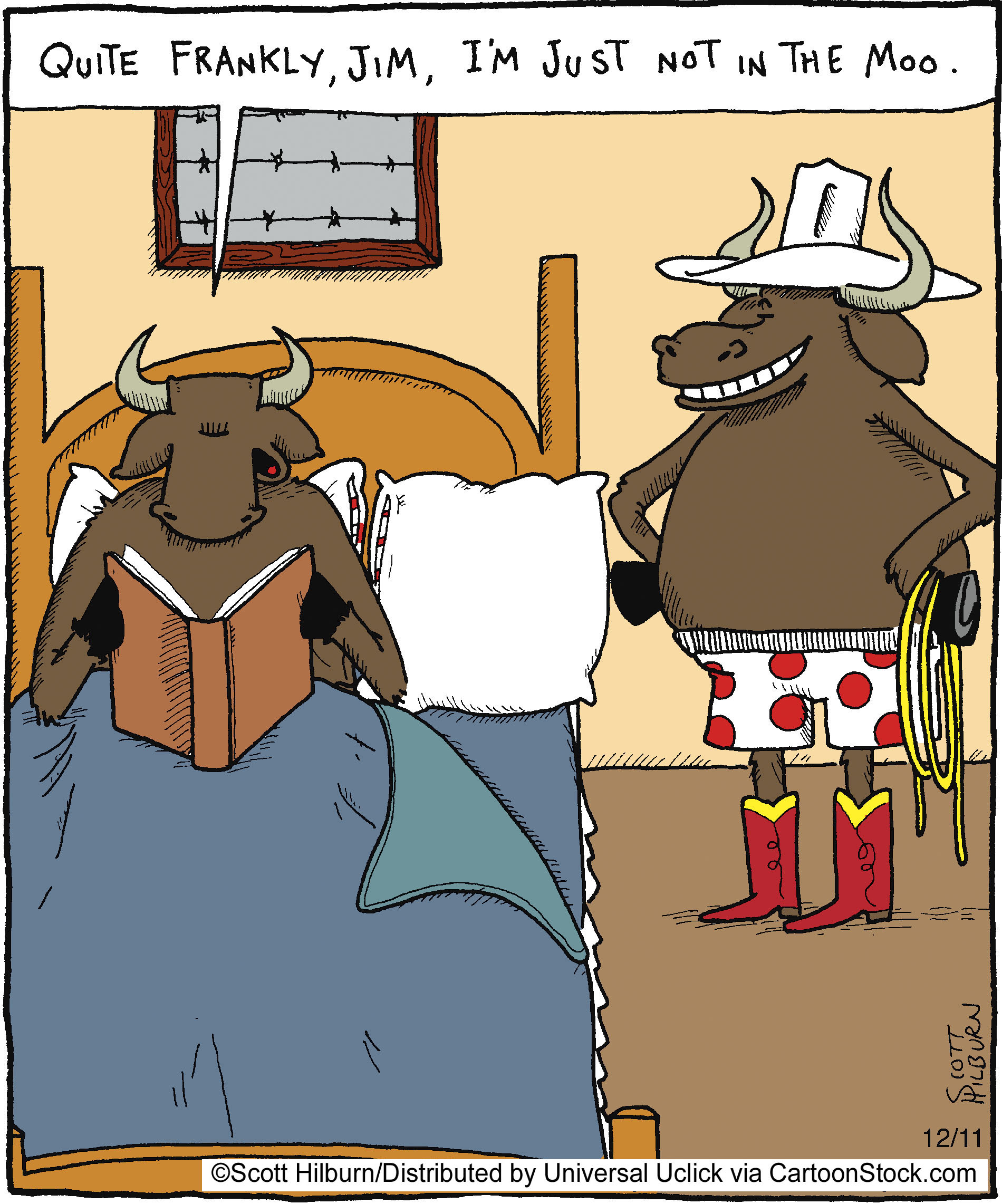
Wednesday Bubble: Are you in the moo? Sex and a sense of purpose
What are we bursting this week? How about midlife and sexual desire. Frankly, I’ve got sex on the brain, sex in midlife, that is. And what we need to do to insure that it continues to be enjoyable, that we desire it and that we please our partners as much as we hope that they please us. Consequently, I am reposting this piece from earlier in the year, with the hope that with a sense of purpose, you’ll become more in the moo. Or mood. Whatever the case may be.
Sexual desire. In midlife, sexual function and sexual desire aren’t well understood, primarily because there are so many factors that enter into equation. This may be why certain silver bullets, like a female viagra, has failed to show any significant improvements in the desire department. And yet, researchers continue to accrue more information about the things that influence desire in women, ranging from the quality of intimate relationships to social support and overall wellbeing. The manufacturer who discovers a pill that addresses all of these will have struck gold. Meanwhile, back in reality, as many as 75% of women in midlife rate sexual health as important enough to warrant further exploration.
Fortunately, we may have another piece of the puzzle: ‘sense of purpose,’ which appears to be associated with greater wellbeing, happiness, life satisfaction, self-esteem, personal growth and optimism. A sense of purpose also appears to improve health, prevent certain diseases and may even improve cognitive function, thereby staving off mental diseases associated with aging. In a study that appears in the online version of Menopause, 459 menopausal women who were sexually active with a partner were followed over three years. Each year, they were asked about their emotional wellbeing (including their general mood, anxiety and depression as well as how often they engaged in and enjoyed sexual activity (specifically desire, type of activity and hugging and kissing). In the final year, they took a test that rated their sense of purpose on a five point scale ranging from ‘there is not enough purpose in my life’ to ‘the things I do are all worthwhile.’
The findings?
A greater sense of purpose equaled a great enjoyment of sexual activities, independent and regardless of other specific life circumstances. In other words, psychosocial functioning, e.g. social support, quality intimacy and overall wellbeing influenced the quality of these women’s sexual lives. On the other hand, menopausal status and use of hormone therapy did not appear to play a significant role in how often women engaged in sex or if they enjoyed it. This is important, as it means that psychosocial wellbeing may ultimately be more important than hormones.
In so far as the desire to engage? Women who were younger, had more social support, felt better about themselves and weren’t suffering from vaginal dryness tended to want sex more than their older peers who didn’t enjoy these factors.
Not surprisingly, many of the factors that researchers stress may help desire and engagement are associated with greater nitric oxide levels, which Dr. Christina Northrup says can help combat sexual dysfunction and improve pleasure.
When it comes to sex in midlife? It may help to think ‘sense of purpose,’ a real sense of purpose, now. (Poetic license, Chrissie!) I’m all for it if improves activity and desire without drugs.
Read MoreWednesday Bubble: Exercise and Sexual Health – How you move affects how you groove. Guest post by Alexandra Williams, MA
Every now and then I like to shake things up in this space, which is why I asked fitness professional writer, speaker and radio host Alexandra Williams (aka @alexandrafunfit on Twitter) to lend me her expertise for a day. What I didn’t expect, however, was for her to rock the sexual health world with the revelation that exercise, i.e. how you move, affects how you groove. Frankly, if all it takes is exercise, you will find me adding an extra hour or so a day at the gym!
Show Alexandra some love. She’s witty and has been putting the fun back into fitness for for some time now…
Image: http://vectorportal.com
Sexual health is defined by Mosby’s Medical Dictionary. as “a capacity to enjoy and control sexual behavior without fear, shame or guilt.” Sexual dysfunction is broadly defined by the Gale Encyclopedia of Medicine as “disorders that interfere with a full sexual response cycle. These disorders make it difficult for a person to enjoy or to have sexual intercourse.”
The good news, especially for older adults, is that most sexual dysfunctions can be treated or alleviated through exercise. It has been found to increase sexual drive, functioning, activity and satisfaction, due to the physical endurance, muscle tone and body composition derived from exercise. In addition, exercise activates the sympathetic nervous system, which encourages blood flow to the genital regions. Even low levels of physical activity can elevate mood and help keep sex organs and muscles in better working condition. A 2000 study found that after just 20 minutes of vigorous exercise, women became more sexually responsive, while men had increased testosterone levels after short, intense bouts of exercise.
Frequency, level of desire, and enjoyment are also affected positively for those who engage in regular exercise, at any age. In 2004, a study of college-age students a strong correlation was found between fitness levels, self-perception, body image, social meaning, outward appearance and sexual performance and desire. These findings were replicated in studies of people in their forties and sixties. And of course, sexual activity itself counts as exercise!
One really interesting comparison of exercise and sexual activity, looked at heart rate and blood pressure during treadmill exercise and sexual activity (not simultaneously)! Unsurprisingly, participants spent more time in sexual activity than they did on the treadmill, but here’s the intriguing point – the treadmill exercise duration predicted sexual activity duration. For each minute of treadmill time, there was 2.3 minute increase in sexual activity duration!
There are also a number of sexual diseases and dysfunctions that are radically improved through exercise. For example, exercise has a protective effect on Type 2 diabetes, with pelvic floor exercises of specific value. A minimum of approximately 50% of overweight men with Type 2 diabetes have erectile dysfunction, a frustrating condition that is helped enormously by cardiorespiratory fitness.
Urinary incontinence is markedly improved via pelvic floor muscle training, with 100% of women reporting decreased incontinence frequency and duration. And it works for men too – after the strengthening training, incidences of urinary and fecal incontinence decreased, and erectile function increased. Pelvic floor exercises are also an effective modality for primiparous (giving birth only once) women who have vaginal deliveries. Desire and satisfaction go up, and pain goes down for these women.
Breast cancer survivors consistently report an improved quality of life (better physical functioning, reduced fatigue and pain) when they participate in physical activity. In addition, prostate and bladder cancer are positively affected by exercise, including its stress-reducing aspects.
Sexual activity itself has been found to help with cardiovascular disease, with researchers finding that sexual activity corresponds to light to moderate physical exercise and entails no significant risk to the majority of patients with cardiovascular disease (severe angina or chronic heart failure are exceptions).
There’s been a lot of research on the relationship between exercise and erectile dysfunction, which affects over 100 million men. The link between cardiovascular disease, metabolic syndrome and erectile dysfunction is strong, and exercise is a mitigating factor on all three. Doctors who prescribe movement to patients with these three issues have reported high success rates. This is good news, especially considering that exercise is a less invasive treatment than medications, surgery or testosterone replacement therapies.
Sexual functioning and health is something everyone should have at any age. Exercise just may be the magic pill!
About the author…
Alexandra Williams, MA, has been in the fitness industry for over 25 years. She is the co-owner of funandfit.org. Together with her twin sister, she writes, teaches and speaks on fitness-related topics, using wit and research! For more, be sure to write to Alexandra and Kymberly at info@funandfit.org.And if you are the sort of person who likes to put a voice to an image, be sure to check Alexandra and Kymberly out on their radio program ‘Fun and Fit.’
Read More
Sex, midlife and a sense of purpose
Sexual desire. In midlife, sexual function and sexual desire aren’t well understood, primarily because there are so many factors that enter into equation. This may be why certain silver bullets, like a female viagra, has failed to show any significant improvements in the desire department. And yet, researchers continue to accrue more information about the things that influence desire in women, ranging from the quality of intimate relationships to social support and overall wellbeing. The manufacturer who discovers a pill that addresses all of these will have struck gold. Meanwhile, back in reality, as many as 75% of women in midlife rate sexual health as important enough to warrant further exploration.
Fortunately, we may have another piece of the puzzle: ‘sense of purpose,’ which appears to be associated with greater wellbeing, happiness, life satisfaction, self-esteem, personal growth and optimism. A sense of purpose also appears to improve health, prevent certain diseases and may even improve cognitive function, thereby staving off mental diseases associated with aging. In a study that appears in the online version of Menopause, 459 menopausal women who were sexually active with a partner were followed over three years. Each year, they were asked about their emotional wellbeing (including their general mood, anxiety and depression as well as how often they engaged in and enjoyed sexual activity (specifically desire, type of activity and hugging and kissing). In the final year, they took a test that rated their sense of purpose on a five point scale ranging from ‘there is not enough purpose in my life’ to ‘the things I do are all worthwhile.’
The findings?
A greater sense of purpose equaled a great enjoyment of sexual activities, independent and regardless of other specific life circumstances. In other words, psychosocial functioning, e.g. social support, quality intimacy and overall wellbeing influenced the quality of these women’s sexual lives. On the other hand, menopausal status and use of hormone therapy did not appear to play a significant role in how often women engaged in sex or if they enjoyed it. This is important, as it means that psychosocial wellbeing may ultimately be more important than hormones.
In so far as the desire to engage? Women who were younger, had more social support, felt better about themselves and weren’t suffering from vaginal dryness tended to want sex more than their older peers who didn’t enjoy these factors.
Not surprisingly, many of the factors that researchers stress may help desire and engagement are associated with greater nitric oxide levels, which Dr. Christina Northrup says can help combat sexual dysfunction and improve pleasure.
When it comes to sex in midlife? It may help to think ‘sense of purpose,’ a real sense of purpose, now. (Poetic license, Chrissie!) I’m all for it if improves activity and desire without drugs.
Read MoreWednesday Bubble: improve your sex life… the maca way
Is Maca (Lepidium meyenil) the Peruvian Viagra?
If you read what’s on the interwebz, you might believe that this Andean plant that is part of the mustard family will improve sexual function and desire. Some clinical studies even suggest that maca can boost sperm count and mobility. Wow. A wonder plant. Makes me all va va va vooommmm; you too?
Um. Not. So. Fast.
I wrote about Maca two years ago and shared some information about studies examining its potential for alleviating symptoms in peri- and postmenopausal women. At the time, I also alluded to its so-called aphrodisiac and energizing properties. Heck, not only is it widely used in Peru but it’s even licensed in Norway for medicinal purposes. So perhaps the claims are true?
Again, not so fast.
I ran across an interesting review of randomized studies on maca that examined its effects on sexual desire and function. Interestingly, of the 88 studies that the researchers identified, only 4 met scientific standards for analysis. All study participants — both men and women — ingested 1.5 g to 3.5 g of Maca daily for up to 12 weeks. Only one of these studies tested dried, natural maca and the rest were commercial grade. Here’s what they learned:
- Despite claims, few scientific trials have evaluated maca’s effect on sexual function.
- Of the few trials that met the researchers’ review criteria, there was only limited evidence to suggest that maca improved desire after at least six weeks.
- None of the studies looked at side effects.
In other words, maca may be useful but it’s still unclear what it’s useful for. Meanwhile, if you want to improve your sexual desire or functioning, you may want to look elsewhere.
Read MoreWednesday Bubble: Will LibiGel liberate testosterone for women?
 Female sexual disorder, also known as hypoactive sexual desire disorder (HSDD, i.e. lack of sexual desire) is big business and the race for the gold ring continues. While the FDA effectively put a halt to the antidepressant flibanseran only months ago, testosterone therapy continues to drive the march towards finding a cure for a low libido. The question remains, however, is this a good or bad strategy? And how about risks and benefits of adjunctive testosterone? Is it safe?
Female sexual disorder, also known as hypoactive sexual desire disorder (HSDD, i.e. lack of sexual desire) is big business and the race for the gold ring continues. While the FDA effectively put a halt to the antidepressant flibanseran only months ago, testosterone therapy continues to drive the march towards finding a cure for a low libido. The question remains, however, is this a good or bad strategy? And how about risks and benefits of adjunctive testosterone? Is it safe?
HSDD is a disorder that robs a woman of her libido and sexual desire. It is believed to affect up to 36% of women between the ages of 20 and 70, although slightly higher numbers of women with some degree of lowered sexual desire have been reported. Especially affected are women who have had their ovaries removed and have entered menopause as a result; these women in particular, have low testosterone levels. Notably, however, not all women who experience diminished sexual desire have low testosterone levels and the cause of HSDD is unknown. In addition to physical causes, relationship and interpersonal/psychological issues are also believed to play a role, making the condition even more difficult to treat. And while testosterone may be helpful for boosting libido, it has also been linked to side effects that include acne, excessive hair loss or growth, hoarseness, weight gain, insomnia, voice deepening and migraines. More importantly, use of testosterone has also been shown to increase cholesterol levels in some women, thereby raising the risk for heart disease.
According to research, the HSDD market ranges from $2 to $5 billion. Even more troubling is the fact that in 2009 alone, physicians wrote more than 4 million prescriptions for testosterone to treat HSDD even though it’s not approved as a therapeutic strategy.
LibiGel® is a topical testosterone gel that is applied to the upper arm. Thus far, it has been shown in short-term, 3 month clinical trials, to significantly increase the number of “sexually satisfying” events by as much as 238% without serious side effects. Since these early trials, the company has been studying over 2,000 postmenopausal women over the age of 50 with an elevated risk for heart disease to observe how well the gel does over the long-term (i.e. 3 years). Thus far, the manufacturer BioSante reports that the rates of reported cardiovascular events and breast cancer are very low and plans to present interim data later this week at this year’s North American Menopause Society Meeting.
Is LibiGel going to liberate sexually dysfunctional women? And what about the other factors that affect desire, such as relationship status, self-esteem, stress and anxiety? Should we be concerned that physicians already prescribe testosterone ‘off-label’ for millions of women and that the company actually reports that over 90% of women using testosterone unapproved for this use would switch to LibiGel once it’s approved?
I am not quite sure if this is an example of irresponsible medicine or an untapped need. I would like to believe that LibiGel might be effective for certain women who have been forced into menopause due to physical conditions. On the other hand, doesn’t the medical treatment of HSDD ignore the obvious: that there are behavioral, social and environmental factors at play that testosterone therapy won’t and can’t address?
What do you think? Is this a bubble to be burst or the “re-desire” revolution? Only time will tell.
Read More