Black cohosh: dose matters
[Image: Thomas L. Muller, The Lady Bird Johnson Wildflower Digital Image Library at the University of Texas, Austin]
I have written frequently about black cohosh on Flashfree. And consistently, the relationship between black cohosh and a decline in certain symptoms has been demonstrated in clinical trials. However, here’s the rub: both formulation and dose appears to matter.
About a year ago, findings from scientifically sound (i.e. randomized, controlled, double-blind) trial demonstrated that taking the higher dose formulation of a black cohosh extract (Ze 450) yielded greater benefits in terms of symptoms severity and quality of life in A group of menopausal women. However, what happens over the long term? Do symptoms reappear or do improvements continue? And, is it really true that dose matters?
In a follow up study, researchers selected over four hundred women with menopausal complaints who were seeing about 100 physicians in general and specialty practices. Initially, these women were treated with a high dose of black cohosh root extract (13 mg) for 3 months and either continued with that dosing for another 6 months or were told by their physician to take a smaller, 6.5 mg dose for 6 months. Overall, a majority of women had moderately severe symptoms (most commonly hot flashes, night sweats, insomnia, anxiety and depression) and about two thirds had received previous treatment for them. Importantly, none of the women taking concurrent hormone therapy were included in the final evaluation.
Over the course of 9 months, black cohosh extract significantly decreased symptom severity by roughly 56% as measured by a scientific menopause scale. More improvements continued to be seen over time, regardless of dose. However, almost 90% of women responded to the high dose extract versus 78% of women responding to the low dose; this suggests that greater benefit can be realized among greater numbers of women with a higher dose. Indeed, women taking the high dose, experienced improved relief of a variety of symptoms (e.g. hot flashes, sweating, dizziness, joint and muscle pain, etc) over time. Both doses were also well tolerated in about 95% of women, although the higher dose was associated with some gastro issues in 12 women).
Another interesting point about this study was that it was conducted in what researchers refer to an ambulatory setting, meaning that it was not a controlled trial situation. Because similar results were observed under controlled conditions, conducting the extension under a more realistic environment allowed them to draw the conclusion that the findings reflected those that would likely be seen in the general population.
The black cohosh extract used in these studies is called Cimefemin® uno (6.5 mg) and Cimefemin® forte (13 mg) and is not available in the States, at least not yet. Meanwhile, if you wish to try black cohosh, read through the archives, speak to your practitioner and used a standardized formulation. It looks like it’s a win-win.
Read More
Newsflash: MsFLASH needs participants
I know, it’s Wednesday and you are probably thinking that I’m taking a mick; who else would be Ms. FLASH than me, right?! However, this is a bonefide ask and post. MsFLASH –Menopause Strategies: Finding Lasting Answers for Symptoms and Health (MSFLASH)– is a network of studies evaluating potentially promising treatments for common menopausal symptoms. Started by the National Institutes of Health, MsFLASH comprises five research centers in Boston, Oakland, Philadelphia, Seattle and Indianapolis who are exploring various interventions for hot flashes, night sweats, mood disorders and sexual issues. Mind you, some of these studies are looking at pharmaceuticals so they might not be appealing. However, if you are a woman between the ages of 40 and 62, going through the pause and experiencing frequent symptoms, you may wish to consider participating.
My goal is and has always been to further our understanding of the challenges of menopause and exploring viable strategies to address them. Without research, this is impossible and leaves only one avenue: hormone replacement. And we all know what a slippery slope that has proven to be.
MsFLASH may ultimately reveal nothing of value. Or, it may be five years times $4.4 million well spent.
Check it out. Who knows? You may be part of history in the making!
Read MoreNewsFlash: ‘First’ Non-Hormonal Treatment for Hot Flashes – Brisdelle
It’s very important when you see news headlines that you read between the lines.
This came across my mailbox earlier in the week:
Noven Receives FDA Approval for Brisdelle™ (Paroxetine) Capsules, the First Nonhormonal Therapy for Vasomotor Symptoms Associated with Menopause
So, let me explain.
Brisdelle is the first non-hormonal treatment for menopause to receive FDA approval. But, it’s not the first nor the only nonhormonal treatment for vasomotor symptoms; heck, one glance at the tag cloud or the archives and you will see that there are lots.
Claim aside, it’s important to break down the news for you.
Brisdelle is a low-dose form of Paxil, an SSRI antidepressant. Because of its dosage, it is only indicated for treatment of hot flashes and night sweats, and not for depression, obsessive compulsive disorder and anxiety.
This is what I wrote late last year when Noven first presented study findings to the North American Menopause Society:
Paroxetine is not the first antidepressant to be studied in menopausal women and you may recall that I wrote about the use of Lexapro for hot flashes about two years ago. You can find that post here. However, paroxetine is the antidepressant that’s all the buzz right now, since Noven Pharmaceuticals presented two studies last week at the North American Menopause Society annual meeting. Note that it’s been reframed as ‘low-dose non-hormonal therapy for menopausal vasomotor symptoms,’ but ya still gotta call a spade a spade and what it is is an antidepressant.
In one of two studies, 568 women (40+ years of age) who experienced 7 to 8 moderate or severe hot flashes on a daily basis of 50 to 60 on a weekly basis took either 7.5 mg of LDMP or placebo daily over six months. By the end of the first month (and in contrast to the study’s start), women who were taking LDMP experienced 28.9 fewer hot flashes per week (compared to 19 fewer per week for women taking placebo pills). By the third month, this increased by roughly 10 fewer per week in both groups. The severity of the hot flashes also significantly decreased. Safety wise, women taking LDMP reported nausea and bronchitis.
In the complementary study, which lasted for three months, 606 women in the same demographic took the same dose of LDMP or placebo. Decreases in mean number of flashes per week were pretty much on par with the first study (33 compared to 23.5 for placebo) and similarly, a trend towards maintaining and growing benefits were observed. Severity of hot flashes also declined but by the study’s end, were not significantly different than placebo. This time, women who took LDMP most frequently reported dizziness and fatigue.
Dr. James Simon, one of the studies’ investigators and a professor of ob/gyn at GWU School of Medicine claims that symptoms of menopause often go untreated when women are unable or unwilling to take hormone therapy, which is not entirely true. Another investigator — Dr. Andrew Kaunitz from the University of Florida College of Medicine in Jacksonville notes that if LDMP is approved by the FDA, “it could be the first nonhormonal option available for women.” Again, this statement is not entirely true. LDMP has the potential to become the first nonhormonal treatment APPROVED by FDA for vasomotor symptoms in menopausal women. There are other options out there but on the most part, they are not embraced by Western practitioners. Take note: while many Western practitioners will argue until they are blue in the face that alternative strategies have no role, are no better than placebo, and do not have evidenced-based trial data to support their use, they are simply incorrect. An unequivocal statement about every alternative strategy available to wo-man is bad medicine at best and at worst? Sheer ignorance.
Back to LDMP…LDMP appears to effectively diminish hot flashes and sweats but it is not without side effects. And while the dosage is considerably lower than full-strength antidepressants, we don’t have enough information to know if it will ultimately mimic its higher dose partner; the most common side effects reported in these trials are the very same that have been reported with Paxil. Another common side effect of Paxil is the effects on libido and it is a well known fact that as many women go through menopause, they experience declines in sex drive, lubrication and the ability to reach orgasm. In the pivotal studies used to gain approval, about half of the women appeared to have sexual dysfunction; what’s unclear is whether or not the cause was the drug or menopause itself. Another important point that is missing from this story is that back in March, the FDA’s advisory committee on reproductive drugs voted against approval, stating that paroxetine’s effectiveness in reducing hot flashes was underwhelming and not unlike that seen among women taking placebo in clinical studies.
I applaud Noven for its efforts to offer an alternative to HRT, one that has been approved by the FDA. However, the way that communications about this agent are being framed, it appears that the spin masters are working overtime. It’s essential to understand that this treatment is non-hormonal but still a pharmaceutical agent. And while I am a huge proponent of antidepressants for depression, I remain skeptical that they are the best agents for addressing menopausal symptoms. Cost may be an issue – no word on the price point as of yet.
I guess that time will tell.
Read More
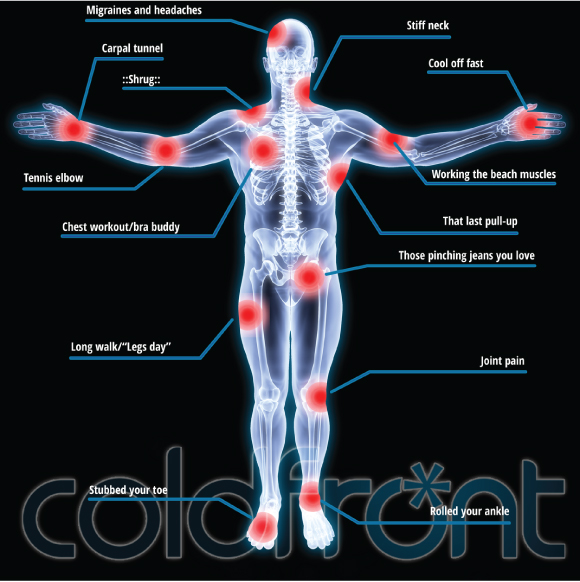
Redefining ‘cool’: Cold Front’s pushing new boundaries
Cold Front ® is not simply for hot flashes any longer. In fact, entrepreneur and Founder of Personally Cool — Susie Hadas — is expanding her horizons and needs your help!
Although hot flashes may be the only game in FlashFree Town, there appears to be a need for cooling outside the menopausal boundaries. And let’s face it; as much as me and several other esteemed menopause bloggers have tried to move the needle, talking menopause is not always easy. And engaging women who want to admit that they’re not simply sweating but flashing can be an upward battle. Consequently, Susie and her team have gone back to the drawing board and emerged with a brand new bag: personally cooling is truly a global endeavour. Voila! A new Indiegogo Campaign has been born! And your assistance is needed!
I can assure you that Susie is not turning her back on menopause but looking forward to help millions of individuals worldwide who suffer from:
- heat intolerance due to multiple sclerosis and thyroid issues
- hormonal changes in men that also cause hot flashes
- chemotherapy side effects
When I caught Susie on the Twitter stream announcing the campaign, I sent her a note asking for more details. She says that when she and her team were on the road, “more people were talking to us – travelers, moms, fashionistas, runners, bikers, hikers, the list goes on. They were all asking us the same question, “Why aren’t you talking to me?” So, she took a step back and decided to relaunch Cold Front on a new level.
Susie notes that in order to grow, they need funding. Moreover, the money they raise to produce another run will enable the company to produce wraps for the gel packs and a single larger gel pack which is what customers have asked for.
And yet, there is another element to this that I want to share with you:
Giving back.
Like many entrepreneurs, Susie has not rested on her laurels or profits and rather, has consistently and continually given back. An attractive aspect of the Indiegogo campaign is that the money that you donate can actually go towards funding three charities whose constituents will benefit from cold therapy:
- Love to Langa, a Cape Townships, South Africa organization that is working to build and renovate Early Childhood Education Centers. Your gift of coldfront® will cool the children down and always be on hand as a non-toxic first-aid solution for minor bumps and bruises.
- Nayaya Health, a Nepal-based organization that provides care to residents of the Achham region of Nepal for free, and employs over 160 Nepalese citizens. (Nyaya Health has been using coldfront® to keep staff and patients cool and aid in pain relief and they have requested more units).
- CT Challenge’s Center for Survivorship, a Connecticut-based survivorship center offering evidence-based programs designed to help empower cancer survivors to live healthier lives.
Susie’s campaign goal is $100,000 and she’s got 35 days left to achieve it.
How about we chip in as a team and cool the world?
Read MoreHot flashes, acupuncture and Traditional Chinese Medicine
Acupuncture continues to top the list of ‘go to’ alternatives for hot flashes. And despite confusion, researchers remain focused on trying to explain (and perhaps overcome) conflicting study findings. That, my dear readers, is a very good thing, as this non-invasive, gentle treatment modality, while not the end all to be all, may one day become as accepted among Western practitioners as pharmaceutical agents are.
The goal of Traditional Chinese Medicine (TCM) and acupuncture as they relate to menopausal symptoms like flashes is to reinforce the kidneys, which according to TCM philosophy, result due to a decline in kidney yin and yang (think: out of balance). As I wrote a few years ago:
TCM and other similar philosophies emphasizes various body systems that together, form a network or grid connected by a meridien, if you will, as well as the relationship of the body to its social and natural environment. Its primary focus on maintaining health and enhancing the body’s ability to fight off disease. TCM will not focus, for example, on treating specific pathogens but rather, on addressing non-specific factors that create disturbances or imbalances within a certain network. TCM also examines how these imbalances may occur in unique parts of a specific system, such as the heart and blood vessels and small intestine (all of which are part of the heart system) and how they change over time. Western medicine, on the other hand, focuses primarily on treating morbidities, or symptoms related to various conditions and diseases. You can read more rabout TCM in this post from September, 2010.
In TCM, menopausal symptoms are believed to be related to a decline in yin or yang in the kidneys. One of the oldest prescriptions in TCM to reinforce kidney energy is known as ‘Qing E Fang’ (QEF) and the first record of its use dates back to the year 960. The preparation is a combination of four key ingredients that are mediated through estrogen receptors and expression, hence, its potential usefulness in menopause. (These ingredients, in case you are interested, are Cortex Eucommiae (whose bark and leaf have an antioxidant effect) Fructus Psoraleae (commonly used for bone health and to treat estrogen associated diseases), Semen Juglandis and Rhizoma Garlic.)
From a Western perspective, there is evidence (albeit preliminary) that suggests that acupuncture actually inhibits the thermoregulatory action of the hypothalmic-pituitary gland that works to create a hot flash. (You can read more about how a hot flash comes about here.) And when study trials are designed with TCM and acupuncture philosophy in mind, they tend to yield positive results – such as a small study that appears online in Menopause journal.
This time, researchers took four groups of women who experienced 20 or more hot flashes a week and assigned them to one of four groups: real acupuncture, sham acupuncture (needles inserted superficially), a 14 herb chinese formulation known as Zhi Mu 14 or a placebo version of the same. Women in all four groups were exposed to licensed practitioners and received TCM diagnoses. An important distinction in this research was that not only did the researchers predetermine 8 standard sites for needle insertion, BUT they also allowed the clinician to use an additional, individual points. In the sham acupuncture group, the acupuncture points corresponded to those used regularly in large clinical trials. Women using the Zhi Mu or the placebo took three capsules daily. And, all women maintained a hot flash and menopause symptom diary.
The findings are intriguing. While Zhi Mu did not appear to have much impact on hot flashes, acupuncture did, resulting in significant improvements in both hot flash frequency and severity as well as in other symptoms. Over the long term, acupuncture also appeared to attenuate bladder and sexual problems as well as joint and muscle aches and pains. Moreover, the findings also suggested that real acupuncture is superior to sham acupuncture in reducing severity and frequency of menopausal symptoms, much more so than other clinical trials. Importantly, the researchers believe that their results, albeit preliminary, are due to standardized plus individualized treatment performed by highly experienced acupuncturists.
Where are the holes? Well, this was a small group of women and Zhi Mu doses were not modified according to individual needs (as they might have been in the real world). They also did not test liver values at the end of the study (evidently Zhi Mu has been linked to liver toxicity in some women) so safety of this particular preparation was not properly assessed. Still, scientific jargon aside, this is what you need to take away from this information:
A very small study that was designed by Western practitioners within the parameters of TCM philosophies once again demonstrated the beneficial effect of acupuncture on hot flashes in particular. When acupuncture is conducted appropriately and by a highly skilled practitioner, positive benefits may be realized.
Before we jump to any future conclusions, it’s time to revisit and consider the value of alternatives for menopausal symptoms. Sometimes a spade simply is not a spade and there is more than meets the eye when you start digging through the details.
Read More
Don’t be cool. Be Super Cool!
 The Japanese lingerie company Triumph has introduced a ‘Super Cool Bra’ to insure that women not only stay cool this coming summer but also keep their electricity bills down. The bra is equipped with removable gel packs that can be placed in the freezer (designed, by the way, to look like a fish bowl), and an attachable ladle so that women can douse themselves with sprinkles of water when the gel packs don’t quite do the trick. There is also a removable fan that can be used any time to boost the chill factor to ‘Super.’ And to complete the package, the bra also includes a sprig of mint and a wind chime to boost other senses that will provide a sense of cool.
The Japanese lingerie company Triumph has introduced a ‘Super Cool Bra’ to insure that women not only stay cool this coming summer but also keep their electricity bills down. The bra is equipped with removable gel packs that can be placed in the freezer (designed, by the way, to look like a fish bowl), and an attachable ladle so that women can douse themselves with sprinkles of water when the gel packs don’t quite do the trick. There is also a removable fan that can be used any time to boost the chill factor to ‘Super.’ And to complete the package, the bra also includes a sprig of mint and a wind chime to boost other senses that will provide a sense of cool.
The point of this neat design is evidently to encourage Japanese consumers to cut down on their electricity consumption during the coming Japanese summer and sadly, the bra will not be massed produced. However, when I first stumbled across this wondrous design, all I could think was ‘menopause.’
Gel packs, ladles, fans – it’s a veritable hot flash bust-er!
Anyone want to bet on the knock-offs? I may need to take a trek to NYC’S Canal Street in search of a Super Duper Cool Bra. Ladle and fishbowl optional!
Happy Friday!
Read More