Depression: the silver lining
I’ve written about depression quite a bit on Flashfree. Not only is age a risk factor among women (with the highest reported levels in women between the ages of 40 and 49) but, the risk of depressive symptoms may be as much as three times higher among women across the menopausal years compared to women who have not yet reached menopause. Moreover, the risk may be more than twice as likely among women who’ve never had depression previously.
However, there is a silver lining: researchers are reporting that in some women, particularly those who experience depressive symptoms for the first time around the time of menopause, depression will eventually dissipate over the eight years following the final menstrual period. In fact, this was proven true in over 200 women whose symptoms were evaluated over a 14 year period around menopause. In this group, depression scores were significantly higher the 10 years before their final period and then decreased roughly 12% per year after their final menstrual period. For women with a history of depression, the odds were not quite as favorable; these women were 13 times likelier to develop depressive symptoms around menopause, and may be as much as 8 times likelier than other women to have recurrences of the blues in the years following the final menstrual period.
The researchers note that women who have greater variability in their levels of FSH — follicular stimulating hormone — may be more likely to develop depressive symptoms during menopause. However, the quicker that these levels change, the more likely a woman is to move past the depression as she gets further into menopause.
The old adage, ‘this too, shall pass,’ may be quite true when it comes to depression during menopause. For women whose history overrides the FSH factor, a reduction in stress, psychotherapy, low doses of SSRIs and a boost in physical activity may help to keep things in balance, especially overall wellbeing.
Read MoreDepression: Walking the Walk
I’m always on the look out for evidence-based alternatives to drug therapy — not because I believe that drugs are bad — but because I believe that sometimes there are safer ways to manage certain conditions, ways that may minimize side effects or interactions. Moreover? We are a society that relies on a quick fix and sometimes, that quick fix brings on a host of other issues.
Depression and hormonal imbalance go hand in hand as much as love and marriage, babies and carriages, and yin and yang. As many as 40% of women are affected by depression during menopause, but there are other factors that come into play, including gender (women are 1.5 to 3 times likelier than men to report a lifetime history of depression), stress, family life, general health issues, a lack of exercise and genetics. Moreover, research has shown that how women perceive the effect of menopause and its symptoms on their physical health can significantly affect whether or not they develop depression at the start of the ‘pause.
When you think ‘depression,’ you probably think melancholy, sadness, feeling blue and out of sorts. But depression can also affect working memory and bring on persistent negative moods, which may not be easily resolved by drugs alone or by behavioral/psychotherapy alone. Consequently, being aware of alternative strategies may be helpful for some people. That’s why I was so intrigued by the concept of Attention Restoration Therapy (ART).
ART examines attention and divides it into two parts:
- Involuntary attention, in which our attention is somehow captured by some sort of stimulus that stands out
- Voluntary or directed attention, which is directed by specific mental processes and intellect
According to ART (which is backed and validated by scientific research) interacting with certain types of environments can promote or invoke involuntary attention; this allows our directed attention a replenishing respite, one that people with depression, who incidentally are more likely to be mentally and attentionally fatigued may benefit. Natural environments in particular, have been shown boost this attention shifting process in healthy individuals. More importantly, a small study that appears in the Journal of Affective Disorders shows that the same benefits may be obtained by clinically depressed persons. In fact, when both women and men were asked to take a 50 to 55 minute walk in an aboretum or an urban setting and deliberately asked to ruminate on a painful memory, they still scored higher on cognitive and attentional testing. After a second walk in an entirely different setting, nature walks were shown to boost both memory and mood.
Mind you, researchers still don’t know how long lasting the effects of nature are on depression, and if it matters if the person actually lives most of the time in a rural or urban setting. However, it does appear that when it comes to depression, walking the walk, especially if it’s in a natural setting, may boost mood and functioning and give attention a much needed rest.
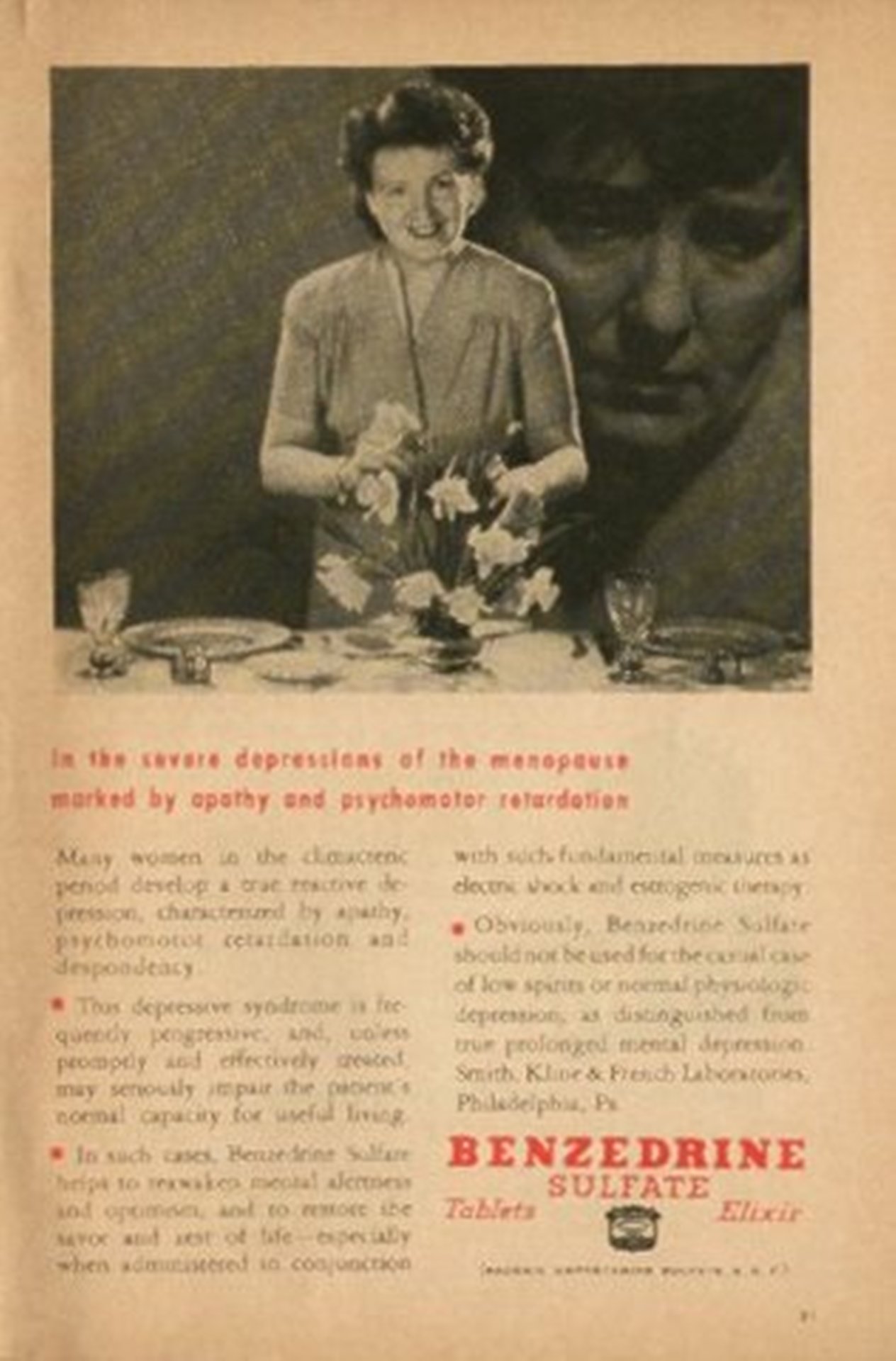
Read More“Severe depression? Apathy? Psychomotor retardation?” How about a bennie?
Every now and then, a post deserves a second viewing. This week, I’m bursting the bubble again on vintage advertising. Nothing like an upper for the mid-week blues, right?
“In the severe depressions of the menopause, marked by apathy and psychomotor retardation…”just use a bennie. You’ll be speeding through your day in no time! (And will probably lose that extra weight too!)
Really! What WERE they thinking?!
Read MoreWednesday Bubble: Depression and midlife – “overmedicalizing” the menopause
What’s the lowdown on depression, midlife and women? And how does the menopause come into play?
I written previously that depression may affect as many as 20% to 40% of women during menopause. However, gender differences in depression evidently begin well before the menopause and women are 1.5 to 3 times likelier than men to report a lifetime history of depression. Moreover, these distinctions start as early as the teen years and continue until the mid 50s, which researchers say, corresponds to female reproductive. Hence, experts have connected waning and altered hormone levels to high rates of mood and anxiety disorders in women.
Is this hypothesis valid? And, where did it originate?
According to a review in the early online edition of the Journal of Affective Disorders, some research has suggested that premenstrual, post partum and menopausal mood disorders are linked and that women are especially vulnerable during certain time periods. This has led to a proposal that reproductive-related depression have its own classification, and that during midlife in particular, all women should be routinely screened for symptoms. Interestingly enough, however, it has also led some researchers to question if we are “overpathologizing the menopause?” Hallelujah! (If you want to read more on medicalizing the menopause, check out one of my favourite Flashfree posts.)
The key finding?
Although studies demonstrate that significant numbers of women in midlife report depressive symptoms, menopause is only one of a range of factors purported to lead to depression during this timeframe. Others include stress, family life, general health issues and a lack of exercise, as well as a history of some sort of anxiety disorder. What’s more is that how women perceived the effect of menopause on their physical health almost doubled the risk that they would first develop depression at the onset of menopause.
The researchers say that although women might score high on self-reported mood scores, these scales or instruments tend to exaggerate the rate of depression in women in midlife and menopause. They also note that if a score is only taken at one time point that is might indicate temporary distress rather than a long-term problem. They add that during menopause, certain symptoms, such as sleep disturbance and fatigue, may be easily confused with depression even though they have nothing to do with a mood disorder and everything to do with hormones.
The bottom line is that symptom overlap and environmental factors can confuse a diagnosis, and that depression is not necessarily more prevalent during menopause than during other periods in a woman’s life. Consequently, like many things, the studies that are out leave more questions than provide definitive answers. Hence, the call for all women to be screened for depression during menopause may be an example of extreme assumption and not based in true necessity.
Is it possible that depression is just the tipping point in the medicalization of menopause?
What do you think?
Read MoreDepression and menopause: can acupuncture help?
Depression and menopause. It keeps coming up as a topic and so I’m going to continue to write about it until researchers find an effective way to battle depression during menopause, effective meaning that it is an acceptable strategy for women who prefer alternatives to pharmaceutical agents, effective in that it addresses the underlying causes of depression in menopausal women, including fluctuating estrogen levels, sleep disturbances, night sweats, hot flashes and life factors, and effective in that it is affordable. It’s a tall order, isn’t it?
As I’ve noted time and again, depression is an important issue for many but not all menopausal women, affecting approximately 20% to 40% in a some way or another. Just this week, I wrote about use of the SSRI antidepressants as an alternative to HRT for hot flashes and depression, and possibly as a stop-gap measure until practitioners more widely embrace alternative strategies. On the heels of this study comes another in the Online Edition of Menopause journal, examining data from one of my favourite studies, ACUFLASH. If you don’t feel like clicking on the link and updates about this study, briefly, in ACUFLASH, researchers randomized 399 postmenopausal women (1 year since last menstrual period) regularly experiencing at least 7 hot flashes daily to acupuncture or no treatment. Moxibustion was used at the practitioner’s discretion and sessions could also be extended by two weeks (from 12 weeks), if needed. Although the practitioners met beforehand to discuss possible diagnoses and recommended treatment points, all treatment was individualized. Both groups of patients also received self care recommendations, which consisted of a one-page information leaflet on care of menopausal symptoms (e.g. soy, herbs, physical activity and relaxation techniques) which they were free to add at their own discretion.
Overall, the mean frequency of hot flashes declined by 48% in women receiving acupuncture compared with 28% of women using self-care methods only. This means that 50% of women receiving acupuncture experienced a 50% or greater reduction in how often their hot flashes occurred, compared to 16% of women using self-care. Significant reductions were also seen in hot flash intensity. Additionally, the acupuncture group reported significant improvements in vasomotor, sleep, and somatic symptoms over the course of the study.
So, what about acupuncture and depression?
In the current study, researchers examined a sample of 72 women who had participated in ACUFLASH and had either received self-care only or self-care plus acupuncture. At the start, almost 31% of these women reported depressive symptoms and of these, about 17% were determined to suffer from moderate to severe depression (based on a scientific method that measures the severity of depressive symptoms). Although these figures are higher than what is normally seen in the general population, severe depression is often seen among women experiencing very frequent hot flashes (7 or more in a 24 hour period for at least 1 week). And while both groups reported significant declines in depressive symptoms during the 12 week study period by as much as 16%, the declines were similar in both groups, indicating the acupuncture,while helpful for lessening the severity of hot flashes, did not have a specific effect on depression.
If acupuncture doesn’t help depression, why did the results indicate such a high level of improvement that under normal circumstances, an individual could forgo drugs for needles?
A key finding of the original and follow up ACUFLASH studies was the feeling of control over symptoms that was imparted by being educated about self-care. However, here’s the rub: even though acupuncture was shown to significantly benefit both the intensity and frequency of hot flashes, it didn’t provide an edge over depressive symptoms compared to self care alone. The researchers say that this leads them to believe that although a domino effect is at-play (i.e. hot flashes lead to sleep issues lead to symptoms of depression) there is something else that also influences the depression part of the equation.
In the interim, it’s frustrating, right? You can deal with your hot flashes but you still feel blue, low, out of sorts. There is clearly a link between the hot flashes and sleep and depression. It simply needs to be teased out a wee bit further. Keep the faith. We’ll get there!
Read More